After rejuvenating procedures, each patient wants to get the desired result as quickly as possible and return to their usual routine of life, without wasting time on rehabilitation and dealing with possible side effects and complications. At the same time, any invasive procedure is stressful for the skin, requires a recovery period and is associated with the risk of adverse events. The discomfort associated with this type of exposure can be minimized by properly preparing the skin for invasive interventions. Svetlana Korkunda, PhD, Associate Professor of the Department of Combustiology, Reconstructive and Plastic Surgery at the Kharkov Medical Academy of Postgraduate Education, told how to do this in an interview for estet-portal.com.
What effect do enzymes have on the skin? What effect do they achieve?
Enzymes in the form that we use in the form of injections are practically no different from our own enzymes that work in our skin. Having studied the capabilities of recombinant enzymes, as well as applying in practice knowledge in the field of biochemistry, normal physiology and pathophysiology, we came to the conclusion that such drugs have many therapeutic and preventive effects when working in different protocols. Thus, substances are introduced from the outside that duplicate the work of the skin’s own enzymes and improve its functioning at the level of its own structures. Speaking about the actual clinical effects, we get a reduction in the volume of adipose tissue on the face and body and tissue tightening.
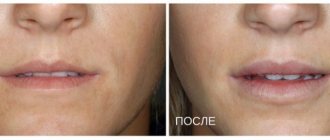
Carrying out invasive procedures on healthy and prepared tissues allows you to shorten the rehabilitation period, obtain a more pronounced result and a long-lasting effect.
How can enzyme therapy prolong the effect of powerful invasive procedures? (H2)
If we talk about the use of three enzymes, then their clinical effect is a reduction in the size of fat cells and an increase in the activity of processes occurring in connective tissue. Thus, further invasive techniques - be it volumetric volumization, threadplasty or a powerful hardware procedure - are used on healthy and prepared tissues, which naturally affects rehabilitation, the severity of the result, and the duration of the effect.
Non-invasive prenatal diagnostics: modern possibilities
The structure of congenital anomalies of the fetus and newborns in the human population is quite stable and fluctuates within 6%: on average, 3% each accounts for major malformations and genetic anomalies. The latter, in turn, fall into three approximately equal groups: chromosomal abnormalities, microdeletion syndromes caused by defects in chromosome sections, and monogenic diseases.
Even 30–40 years ago, the basic criterion for a high risk of aneuploidy was only the age of the mother, which was the basis for the recommendation to undergo an invasive diagnostic test that determines the karyotype of the fetus. Such examinations include transabdominal chorionic villus aspiration, placentocentesis, cordocentesis, and amniocentesis. However, significant concerns were raised by the increased risk of complications during the collection of biomaterial - a number of studies estimate the risk of pregnancy loss at 1%.
To improve diagnosis, in 1997, the first trimester screening, which is still in use today and is considered the most informative, or a combined test with a sensitivity of up to 90% for identifying Down syndrome (DS) was developed with 5% of false positive results (FPR). Despite its effectiveness, the specificity of the test has prompted the development of other, more comprehensive noninvasive testing methods.
The most modern of them are based on the isolation and study of fetal DNA freely circulating in the blood plasma of pregnant women and make it possible to narrow the range of indications for invasive techniques. The technology of non-invasive prenatal testing (NIPT) is based on the long-known phenomenon of the presence in the peripheral blood of pregnant women of a small number of fetal cells containing such DNA (1/105–1/106 of maternal nuclear cells), which pass through the placental barrier.
New opportunities opened up in the late 1990s, when fetal free DNA (ffDNA) was isolated from the blood plasma of pregnant women. Its source is believed to be placental cells that have undergone apoptosis, as well as fetal cells that penetrate the fetoplacental barrier.
The amount of fetal DNA is relatively small (according to various sources, from 0.4 to 11.4% of the total DNA in blood plasma) and depends on the duration of pregnancy. On average, by the fifth week, the concentration of ffDNA is already possible for analytical detection and further study of the genetic status of the fetus.
The rapid development of NIPT techniques in the 2010s has led to a significant expansion of the range of detected pathologies and a significant increase in the accuracy of tests. Thus, meta-analyses of recent years (2014–2017), summarizing clinical studies on the use of NIPT, indicate that the detection efficiency when using NIPT for trisomies on chromosomes 21,18,13 is 99.7; 98.2 and 99% retrospectively with a total false positive rate of 0.13%.
In general, the non-invasive test is considered to be 10 times more effective than biochemical screening. But at the same time, as mentioned above, almost 100% reliability is noted only when diagnosing trisomy 21 chromosomes (SD), and for other chromosomal disorders it ranges from 92 to 97%.
Due to its high sensitivity and the ability to accurately detect a number of aneuploid and other pathologies, as well as potential Rh conflict, non-invasive prenatal testing has become part of the first trimester screening protocol in a number of countries. In particular, in the UK, since 2020, the National Screening Committee has recommended incorporating NIPT into the existing government program for detecting fetal anomalies and testing women with an increased risk (> 1: 150) of aneuploidy (based on the results of a combined test).
Approximately the same recommendations apply in Sweden. In France, where all genetic testing in pregnant women, including invasive ones, is covered by the public insurance system, circulating fetal DNA testing is recommended for women at increased risk based on first trimester screening (from 1:1,000 to 1:51). High-risk pregnant women (>1:50) are advised to undergo invasive diagnostics, but may undergo molecular screening first.
In general, three basic NIPT approaches are practiced in the world today:
- a non-invasive genetic test is used as a primary test before conducting a detailed ultrasound as part of a combined screening of the first trimester of pregnancy;
- Based on the results of combined traditional screening, high, medium and low risk groups are formed. In this case, free fetal DNA is detected in patients with average risk;
- Groups of high-risk pregnant women informed by the doctor who independently decide to undergo NIPT before the recommended invasive intervention. This option is used today in Russia and partly in the USA.
The practice of the REMEDI reproductive clinic has gained successful experience in using such NIPT techniques as Prenetix. In laboratory conditions, extracellular DNA is isolated, which is studied by sequencing using a special algorithm.
The method, in addition to determining the sex of the child, allows you to accurately and safely identify the most common chromosomal pathologies:
- Down syndrome (disease incidence 1: 700);
- Klinefelter syndrome (disease incidence 1: 700);
- Shereshevsky-Turner syndrome (disease frequency 1: 1,500);
- Edwards syndrome (disease incidence 1: 6,000);
- Patau syndrome (disease incidence 1: 7,000);
- an increase in the number of X chromosomes in girls and Y chromosomes in boys (disease frequency 1: 1,000).
Thus, the non-invasive prenatal test is absolutely safe, highly informative and recommended for use in pregnant women of different risk groups.
How do you assess the prospects for the use of enzyme therapy in aesthetic medicine?
The more I work with enzymes, the more opportunities and prospects I see for their use. If we started working exclusively in the context of local effects on adipose tissue, and then on scar tissue, then today protocols have been developed for use in rehabilitation regimes for patients after invasive procedures, for example:
- Aptos threadplasty;
- volumization with fillers;
- some surgical interventions;
- in the presence of inflammatory processes.
Therefore, the prospects for using enzyme therapy are quite large; the main thing is to understand the principle of action of products in tissues and receive the correct information not only from representatives, distributors and manufacturers, but also from independent sources, for example, textbooks on biochemistry and human physiology.
Share:
Invasive ventilation
An endotracheal tube is inserted into the trachea through the mouth or nose and connected to a ventilator.
With invasive respiratory support, the ventilator provides forced pumping of oxygen to the lungs and completely takes over the breathing function. The gas mixture is supplied through an endotracheal tube placed into the trachea through the mouth or nose. In particularly critical cases, tracheostomy is performed - a surgical operation to dissect the anterior wall of the trachea to insert a tracheostomy tube directly into its lumen.
Invasive ventilation is highly effective, but is used only if it is impossible to help the patient in a more gentle way, i.e. without invasive intervention.
Who needs invasive ventilation and when?
A person connected to a ventilator can neither speak nor eat. Intubation is not only inconvenient, but also painful. Because of this, the patient is usually placed in a medically induced coma. The procedure is carried out only in a hospital setting under the supervision of specialists.
Invasive ventilation is highly effective, but intubation involves placing the patient in a medically induced coma. In addition, the procedure is associated with risks.
Traditionally, invasive respiratory support is used in the following cases:
- lack of effect or intolerance of NIV in the patient;
- increased drooling or production of excessive sputum;
- emergency hospitalization and the need for immediate intubation;
- coma or impaired consciousness;
- possibility of respiratory arrest;
- presence of trauma and/or burns to the face.
How does an invasive ventilator work?
The operating principle of devices for invasive ventilation can be described as follows.
- For short-term mechanical ventilation, an endotracheal tube is inserted into the patient's trachea through the mouth or nose. For long-term mechanical ventilation, an incision is made in the patient's neck, the anterior wall of the trachea is dissected, and a tracheostomy tube is placed directly into its lumen.
- A breathing mixture is delivered through a tube into the lungs. The risk of air leakage is minimized, so the patient is guaranteed to receive the right amount of oxygen.
- The patient's condition can be monitored using monitors that display breathing parameters, the volume of supplied air mixture, saturation, cardiac activity, and other data.
Features of equipment for invasive ventilation
Equipment for invasive ventilation has a number of characteristic features.
- Completely takes over the breathing function, i.e. actually breathes instead of the patient.
- It requires regular checking of the serviceability of all valves, because... The patient’s life depends on the performance of the system.
- The procedure must be supervised by a doctor. Weaning the patient from the ventilator also requires the participation of a specialist.
- Used with additional accessories - humidifiers, cough cleaners, spare circuits, suction units, etc.
Nurses were prohibited from performing certain procedures in cosmetology
A cosmetology nurse performs preventive, therapeutic, rehabilitation measures and procedures only prescribed by a cosmetologist. The nurse can carry out these procedures using drugs and devices, the instructions of which indicate that they can be used by nursing staff.
There is a clear prohibition in the new Order. A nurse does not have the right to independently provide services, without a doctor’s prescription and using drugs and devices, in the instructions of which the requirements for a specialist are designated as “a specialist with a higher medical education.”