- Department of Plastic Surgery
Department of Plastic Surgery » - Center for Reconstructive Plastic Surgery
Center for Reconstructive Plastic Surgery »
- Articles by our doctors
Articles by our doctors »
- Autologous fat grafting in reconstructive breast surgery
Scientific and practical journal “Povolzhsky Oncological Bulletin”, 2015. No. 3, pp. 4-8
The author of the article is Semyon Igorevich Fedosov, reconstructive plastic surgeon at the RAMI clinic.
Introduction
Lipofilling (autotransplantation of fat) is the correction of body contours by transplanting autogenous adipose tissue from the donor area to the recipient area using injections.
The use of autogenous adipose tissue is possible for any conditions that are characterized by atrophy or defect of subcutaneous adipose tissue, as well as if the patient wishes to change the contour of a particular part of the body.
There is no need to talk about the advantages of your own tissue over synthetic injectable materials or implants. The use of adipose tissue in reconstructive plastic surgery has been known for a long time; in 1883, Neuber first proposed the idea of transplanting the patient’s own adipose tissue to replace the volume of subcutaneous soft tissue. In 1889, Van Der Meulen used the greater omentum, removed during surgical treatment of a diaphragmatic hernia, as a fat graft. T. Czerny in 1895, performed breast augmentation through lipoma transplantation. Lexer in 1920 performed breast augmentation using fat pads as a filler. Erich Lexer also owns a two-volume treatise, Die Freien Transplantationen (free transplantation), published in 1919, containing almost 300 pages on the technique of fat tissue transplantation. However, by this time the disadvantages of fat tissue grafting had already been noted. Thus, F. Verderame noted that the transplanted fat has a tendency to be reabsorbed, and therefore recommended transplantation with hypercorrection. And in 1925, Davis and Traut published data on methods for increasing the effectiveness of fat tissue transplantation. In 1929, O. Loewe proposed including dermis in the fat graft, which, according to the author, not only gave it density, but also provided better vascularization. By the beginning of the 40s of last year, the number of works devoted to the problem under study increased. Errors and complications were analyzed, new methods of using fat were proposed, and a study was carried out on the speed and volume of fat loss after transplantation. Bames in 1953 reported on the possibility of breast augmentation using the patient's own adipose tissue as a filler. Of course, the result of these “experimental” operations was unsatisfactory, because At that time, there was no modern understanding of the anatomical and physiological properties of adipose tissue. The first publication reflecting retrospective results of the use of adipose tissue in plastic surgery of the mammary glands dates back to 1987 and is devoted to the “microinjection technique of mammary gland augmentation using lipoaspirate obtained after liposuction” (Bircoll et al). In 1988, the American Society of Plastic Surgeons published an article, “Banned the Procedure,” which detailed the “dark side” of autologous fat grafting and described the technique as “flawed.”
However, the accumulation of experience and knowledge in the field of using adipose tissue as a plastic material and the definition of the lipografting procedure from the perspective of transplantology made it possible to formulate a modern and effective concept of using a fat graft.
Transplantation of one's own adipose tissue, as a separate technique for breast reconstruction, was described in 2000 in the article “Reconstruction after mastectomy and lumpectomy; Delay/ Rigotti.” However, in the same year, a work was published: “the method of fat tissue transplantation is good as an addition to breast reconstruction, unsatisfactory as a method of primary reconstruction...” (American Society of Plastic Surgeons), which describes in detail and justifiably a number of unsolved problems that limit the use of this techniques as a mono-tool for reconstructive surgery of the mammary glands.
Currently, research is ongoing into the dependence of the survival rate of adipocytes on the technique and area of fat harvesting. A search is underway for a universal donor area. Morphological studies of the transplanted adipose tissue are carried out and the degree of its resorption is determined. The process of fat graft vascularization and its effect on the survival rate of transplanted adipocytes is being studied. Methods for pre-injection treatment of adipose tissue are being developed in order to increase its viability. Despite great achievements in these areas, many issues still remain unresolved.
So, taking into account all of the above, the question naturally arises: “Has the role and consistent method of fat tissue transplantation been determined?” Is it possible to widely and actively use this technique? All of the above suggests that it is necessary to clearly formulate the indications, contraindications and target audience of patients for whom the lipofilling method is not only possible, but also safe.
Based on the information received, our center began active work to introduce this technique into clinical practice.
Main part
The use of adipose tissue in reconstructive plastic surgery has been known for a long time; in 1883, Neuber first proposed the idea of transplanting the patient’s own adipose tissue to replace the volume of subcutaneous soft tissue. In 1889, Van Der Meulen used the greater omentum, removed during surgical treatment of a diaphragmatic hernia, as a fat graft. T. Czerny in 1895, performed breast augmentation through lipoma transplantation. Charles C. Miller of Chicago, a birth defects specialist, expressed his positive views on the concept of fat grafting in his book Cosmetic Surgery: Correction of Congenital Defects. Following the example of Czerny, A. Bier in 1910 used adipose tissue from a removed lipoma to correct facial hemiatrophy. Lexer in 1920 performed breast augmentation using fat pads as a filler, and he also used this method to correct atrophic scars in the periorbital area, noting that the technique not only serves to fill the defect, but also prevents re-fixation of the skin to the bone by scar tissue fabrics. Erich Lexer also owns a two-volume treatise, Die Freien Transplantationen (free transplantation), published in 1919, containing almost 300 pages on the technique of fat tissue transplantation. However, by this time the disadvantages of fat tissue grafting had already been noted. Thus, F. Verderame noted that the transplanted fat has a tendency to be reabsorbed, and therefore recommended transplantation with hypercorrection. Since the 20s of the last century, a large number of works have been published on fat tissue transplantation. Louis Placide Mauclaire in 1922 (Paris) published the monograph “les Greffes Chirurgicales”, which summarized the experience of fat transplantation around the tendons of the hand to restore tissue glide and transplantation of the greater omentum to close a large bladder defect. And in 1925, Davis and Traut published data on methods for increasing the effectiveness of fat tissue transplantation. Charles C. Miller in 1926 proposed the syringe method of fat tissue transplantation for the correction of nasolabial folds, periorbital area and saddle nose. In 1929, O. Loewe proposed including dermis in the fat graft, which, according to the author, not only gave it density, but also provided better vascularization. By the beginning of the 40s of last year, the number of works devoted to the problem under study increased. Errors and complications were analyzed, new methods of using fat were proposed, and a study was carried out on the speed and volume of fat loss after transplantation. In 1940, Lyndon A. Peer wrote in his writings: “...fat grafts lose approximately 45% of their mass and volume after 1 year.” Bames in 1953 reported on the possibility of breast augmentation using the patient's own adipose tissue as a filler. Of course, the result of these “experimental” operations was unsatisfactory, because At that time, there was no modern understanding of the anatomical and physiological properties of adipose tissue. Since the 80s of the last century, many authors have reported on the successful use of autologous adipose tissue in the correction of facial wrinkles, aging hands, etc. The first publication reflecting retrospective results of the use of adipose tissue in plastic surgery of the mammary glands dates back to 1987 and is devoted to the “microinjection technique of breast augmentation.” glands using lipoaspirate obtained after liposuction” (Bircoll et al). In 1988, the American Society of Plastic Surgeons published an article, “Banned the Procedure,” which detailed the “dark side” of using autologous fat tissue and defined the technique as “vicious.”
However, the accumulation of experience and knowledge in the field of using adipose tissue as a plastic material and the definition of the lipografting procedure from the perspective of transplantology made it possible to formulate a modern and effective concept of using a fat graft. In the late nineties, Aiache and a number of other authors reported positive long-term results of lipografting. Nechajev pointed out the need to separate the resulting aspirate in order to separate the active fat portion from the blood, supernatant and oil. He reported 40-50% adipocyte survival. The scope of application of lipofilling in aesthetic surgery has expanded (Adant J., Bluth F., 2000). In 1989, Abel Chajchir reported a 90% success rate for fat grafting. Based on the experience of fat tissue transplantation in 500 patients, he formulated his concept of this technique: a ban on the use of local anesthetics; gentle sampling of adipose tissue; ban on fat washing; injection of lipoaspirate in three layers: skin, fascia, muscle.
In 1994, Carpaneta published the results of the dependence of the resorption of transplanted fat on the volume of injected tissue. His research showed that the thickness of the fat graft should not exceed 3 mm. The culmination of almost 80 years of research into fat tissue transplantation was the work of Coleman SR, which essentially became the basis of the modern method of transplanting one’s own fat tissue. In the 1990s, Sidney R. Coleman generalized the lipografting technique. He pioneered the use of multi-level cross-injection of fat grafts. He also recommended centrifuging the lipoaspirate before its administration in order to divide the resulting graft into the necessary fractions during collection. His concept of effective fat engraftment was as follows:
1) It is necessary to use blunt-ended cannulas with a diameter of no more than 17 mm, connected to a 10 ml syringe for collecting fat;
2) Lipoaspirate must be purified to specific, strict technical specifications;
3) The injection of fat should be performed with microgranules to increase the area of contact of the graft with surrounding tissues and improve diffuse trophism of adipocytes until revascularization occurs. The culmination of his work on fat tissue transplantation and the achievement of lasting results after this procedure were the works “Structural Fat grafting” in 2004 and “Fat injections: from filling to regeneration” in 2009.
Due to the widespread introduction of adipose tissue transplantation into clinical practice, new methods and algorithms for the collection, processing and injection of fat are being developed. So Dr. Pierre F. Fournier proposed a new method of vacuum aspiration of adipose tissue using disposable Felman canulas. This cannula allows for the harvesting of individual columns of adipose tissue while minimizing damage to adipocytes, which helps ensure long-term aesthetic results. Since individual columns of adipose tissue are collected, there is no need to centrifuge the lipoaspirate, which reduces surgical time. However, this method of harvesting adipose tissue is very aggressive in relation to donor areas, and, as a rule, is accompanied by quite pronounced hematomas in the postoperative period. Also, the use of a monoblock method of sampling adipose tissue is possible only in patients with a sufficiently pronounced fat depot. The use of lipografting in aesthetic facial surgery is considered in the concept of “volumetric rejuvenation”. Despite the fact that tissue augmentation through fat injection has been used for more than 100 years, the search for optimal methods is still ongoing. One of Roger Amar's techniques is called "autogenous fat injection" (AFI) aimed at achieving the most long-lasting aesthetic results. This technique involves injecting centrifuged fat into or directly next to the facial muscles. This method is based on the work of Guerrosantos, who in 1996 proved the five-year persistence of fat in the muscle tissue of rats.
Most volume grafting procedures using adipose tissue are aimed at replacing lost subcutaneous fat. However, as we age, all facial tissues undergo atrophy: fat, muscle, bone. Significant loss of subcutaneous fat can lead to noticeable age-related changes. Coleman and others have described a flattening of the facial contour due to fat loss.
IMAGE is indicated for patients with reduced facial tissue volume, but sufficient skin elasticity. In this procedure, fat is not used to fill deep wrinkles. The method involves restoring muscle volume, contours and function. Of the individual areas of the face, the lower third most often needs correction. Restoration of this area can be performed using IMAGE, replenishing lost lip volume, adding volume to the chin and emphasizing the edge of the lower jaw. In the periorbital region, IMAGE can be used to restore a deformed tear trough. The procedure is also ideal for post-facelift patients whose neck appears skeletonized. IMAGE is not suitable for patients with significant skin laxity, very deep nasolabial folds and ptosis of the cheeks and neck.
IMAGE involves the injection of a small amount of fat along the well-vascularized bed of the facial muscles. Injecting fat along the muscle enhances its function, which is used in various fields of medicine, for example in otorhinolaryngology, urology and gastroeterology, when fat is injected into weak vocal cords or sphincters for therapeutic purposes. Due to fat, not only the thickening of the muscle bundle occurs, but also the hypertrophy of the muscle tissue itself. Correcting volume and enhancing muscle function during IMAGE provides a facelift, giving it the contours characteristic of a young age.
Recently, in the literature, along with reports concerning the use of adipose tissue as a kind of “filler” or plastic material, works have appeared devoted to the use of autotransplantation of adipose tissue enriched with stromal vascular cell fraction (SVCF), obtained using the classical P. Zuk method - “manually” » – in the laboratory, where lipoaspirate is supplied immediately after surgery; Cytori Celution device since 2008 and GID SVF-1.
Intact adipose tissue is a vascular, self-renewing structure consisting of adipocytes, a stromal vascular cell fraction (SVCF), and a supporting fibrous stroma. SVCF is a unique cellular complex containing adipose tissue stem cells - SCAT (which are a key component of SVCF), endothelial and smooth muscle cells of blood vessels and their precursors, pericytes, fibroblasts, blood cells, including B and T lymphocytes. It should be noted that adult adipose tissue is the richest in stem cells compared to other sources (in particular, 1 cm3 of this tissue contains 100–1000 times more stem cells than 1 cm3 of bone marrow). The positive effect of SVCF on reparative processes in the transplantation area is due to the cumulative interaction of stem cells that are part of SVCF. This feature of adipose tissue stem cells is based on significant endocrine activity (FGF-fibroblast growth factor, VEGF-vascular endothelial growth factor, TGFb-transforming growth factor, IGF-insulin-like growth factor, PDGF-platelet growth factor), as well as the ability of the latter to carry out neoangiogenesis and adipocyte regeneration. Unlike adipocytes, the cells that make up the SVCF are resistant to oxygen deficiency. Moreover, according to H. Suga and H. Thangarajah (2009)[13], hypoxia helps stimulate the differentiation of SCAT in the angio- and adipogenic directions. Thanks to this, during the first 2–3 months after transplantation of the SVCF-enriched lipograft, its renewal is observed, which, accordingly, significantly improves its quality.
Transplantation of one's own adipose tissue, as a separate technique for breast reconstruction, was described in 2000 in the article “Reconstruction after mastectomy and lumpectomy; Delay/ Rigotti.” However, in the same year, a work was published: “the method of fat tissue transplantation is good as an addition to breast reconstruction, unsatisfactory as a method of primary breast augmentation...” (American Society of Plastic Surgeons), which describes in detail and justifiably a number of unsolved problems that limit its use this technique as a mono-tool for reconstructive and aesthetic surgery of the mammary glands. In reconstructive surgery of the mammary glands, such tasks are: deficiency of recipient capacity; fibrous changes in the area of interest after radiation therapy; lack of skeletal properties in adipose tissue. The main obstacles to the use of one's own adipose tissue as a monomethod for primary mammary gland augmentation is the shortage of donor and recipient areas, because Most patients seeking treatment for breast enlargement have an asthenic body type. One of the solutions to the problem of deficiency of recipient zones during primary augmentation and reconstruction of mammary glands through lipografting is the use of external tissue expanders. As an example of the technique of using adipose tissue in combination with external tissue expansion in reconstructive plastic surgery of the mammary glands, see Roger Khouri in 2002. A system for reconstruction and augmentation of mammary glands with own fat, based on the principles of tissue engineering in vivo. The BRAVA system is a modified external expander that produces a gentle three-dimensional stretching effect. As a result, the glandular tissue hypertrophies. The tissues are more intensively supplied with blood, creating favorable conditions for the engraftment of fat grafts.
Research into the metabolism of adipose tissue in vivo and in vitro is currently ongoing. The dependence of the degree of adipocyte survival on the technique and area of fat harvesting is studied. A search is underway for a universal donor area. Morphological studies of the transplanted adipose tissue are carried out and the degree of its resorption is determined. The process of vascularization of the fat graft and its effect on the survival rate of transplanted adipocytes is being studied. Methods for pre-injection treatment of adipose tissue are being developed in order to increase its viability. Despite great achievements in these areas, many issues still remain unresolved.
So, taking into account all of the above, the question naturally arises: “Has the role and consistent method of fat tissue transplantation been determined?” Is it possible to widely and actively use this technique? All of the above suggests that it is necessary to clearly formulate the indications, contraindications and target audience of patients for whom the lipofilling method is not only possible, but also safe. Based on the information received, our center began active work to introduce this technique into clinical practice.
Materials and methods
From June 2014 to July 2020, we performed 54 operations aimed at correcting the shape and volume of the mammary glands through fat tissue transplantation. All patients underwent careful selection and all had clear indications for the specified surgical treatment. Lipografting was not used in immunosuppressed patients or those scheduled for radiation therapy. In all cases, lipografting was used as an additional technique to the main reconstructive plastic surgery.
The main goals of using lipografting as an additional technique were: 1) increasing the projection; 2) filling the upper slope; 3) restoration of symmetry; 4) adding volume to the mammary glands after reconstructive operations using full-thickness complex autografts (flaps).
The main way to achieve these goals was to solve the following problems.
1. Obtain a sufficient volume of lipoaspirate. 2. Correlate the volume of lipoaspirate with the reserve capacity of the recipient zone. 3. Select the introduction layer. 4. Determine the frequency of operations.
Based on the principles of transplantology, the following stages of lipografting can be determined:
1) Determination of the zone of interest (recipient zone);
2) Selection of donor area. Preference is given to areas with a sufficient amount of fat: paraumbilical area, abdominal flanks, inner thighs, riding breeches, back, shoulders.
3) Anesthesia. Depending on the volume of fat taken and the number of donor areas, we use local anesthesia with intravenous potentiation or ETN. To collect fat, a tumescent technique is used: Sol. Lidocaini 10%-1ml+ Sol. NaCl 0.9%-400ml+ Sol. Adrenalini 0.5 ml. To prevent flooding of adipocytes, we abandoned the use of glucose and bicarbonate in the solution;
4) Fat removal. To obtain lipoaspirate with the maximum number of living adipocytes and minimize the content of blood in the lipoaspirate, we use: delicate cannulas, minimal vacuum (up to 0.6 bar), minimal aggression in the donor area;
5) Preparation for introduction. After taking the fat, the latter is centrifuged for 1.5 minutes at 1300 rpm; This ensures minimal contact of lipoaspirate with air, minimal transfer from system to system;
6) Introduction of fat. To inject fat, we use the micro-grafts technique, layer-by-layer retrograde injection without resistance. Hypercorrection is unacceptable, because The greater the volume of fat, the higher the risk of liponecrosis. At the introduction stage, strict adherence to the FTF (fat to fat) and FTM (fat to muscle) principles. To determine the permissible volume of transplanted fat into the recipient area, we are guided by the concept of “recipient capacity”; the amount of transplanted fat in one horizontal layer is limited by the capacity of 2 mm channels and the need to maintain no less distance between them, so as not to compromise the vascularization of the recipient bed. The boundaries of the injection zone can be expanded if lipofilling is carried out not in one, but in two or more tiers. You just need to remember that the vertical distance between the layers should be sufficient to maintain the same vascularized layer of recipient tissue between them;
7) Volume distribution.
All stages of the operation are aimed at improving the survival of fat.
In the postoperative period, bandages were applied to the puncture sites and antibiotic therapy was prescribed for two days. In this case, cold, pressure and massage of the recipient area were completely excluded.
Example #1:
Patient O., 33 years old. Diagnosis: cancer of the right breast, condition after complex treatment in 2012. BRCA mutation. Condition after bilateral subcutaneous mastectomy with simultaneous reconstruction with implants. Ripping in the area of the upper slope of the right breast.
Rice. 1 (a,b)
Example #2:
Patient X. 40 years old. Diagnosis: cancer of the left breast. Condition after complex treatment in 2013. Condition after subcutaneous mastectomy on the left with simultaneous reconstruction with an implant in combination with TDL, prophylactic subcutaneous mastectomy on the right with simultaneous reconstruction with an implant dated July 26, 2013. Deficiency of the upper slope of the mammary glands, cicatricial deformation of the lower slope of the right mammary gland.
Rice. 2 (a,b)
Depending on the clinical case, patients underwent one to three lipografting sessions. It should be noted that over the eleven-month follow-up period, the loss of adipose tissue in the recipient area ranged from 0 to 30%.
Model of engraftment of transplanted fat
Some early studies demonstrated that virtually all transplanted mature adipocytes are able to retain their properties at the recipient site. Jones et al. have clearly shown in vitro that fat collected with a syringe under low vacuum remains metabolically active and viable.
In addition, given the fact that autologous fat grafts engraft best where homogeneous adipose tissue exists, it is considered highly likely that additional stimuli in the form of growth factors will only facilitate this.
Later studies showed that placing PRP in cell culture also contributed to the restoration of damaged cytoplasmic membranes to an intact, metabolically active state. In addition, it turned out that these growth factors act on stem cells located in adipose tissue and promote their transformation into mature adipocytes.
Autologous fat collection using a low-pressure syringe
Most experienced plastic surgeons use a low-pressure syringe to collect fat.
Selecting a donor site for fat harvesting is an important step. Autologous fat grafts have been shown to exhibit donor site memory, meaning they can retain the metabolic characteristics of donor site adipocytes. This has important clinical implications for selecting ideal donor sites, making such selection not based on convenience or surgeon preference, but on the metabolic activity of fat in the individual patient.
Before fat collection, donor areas are infiltrated with Klein's solution, this ensures bloodless graft collection. Currently, superpolished cannulas with an outer diameter of 2.1–3.7 mm are used.
After washing the fat, PRP is added to it in an approximate ratio of 0.5–1% of the total volume of the graft prepared for transplantation. After the graft and PRP are thoroughly mixed, they are allowed to sit for 5 to 10 minutes to allow the release of growth factors from the platelets. Only after this the fat, enriched with growth factors, is ready for transplantation into the recipient area (breast).
Breast augmentation using autologous fat grafting enriched with PRP
As with breast augmentation with implants, with this method, markings are made immediately before the operation. A point is marked in the inframammary fold through which the graft will be inserted.
Typically, fat is injected between the pectoralis major muscle and the gland and between the gland and subcutaneous fat. Intramuscular or axillary transplantation is also possible. As in the case of small volume fat transplantation, in the case of platelet-rich plasma fat transplantation, it is necessary to inject it evenly in small doses in several layers.
Currently, a fat transfer volume of up to 300 ml per breast is considered normal. It is very important to understand that the volume of graft that can be transplanted is directly related to the existing volumes of native fat. That is, in patients with a large amount of their own fat in the breast, larger volumes can be transplanted. And very thin patients or patients with almost imperceptible retroglandular fat deposits may not be ideal candidates for large-volume fat grafting.
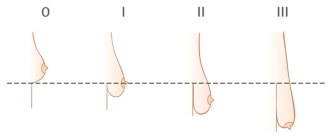
The average increase in breast volume with this technique is approximately one cup size, with some patients experiencing greater increases. With this technique, grafting options are available to deal well with minor asymmetries, as well as for filling the upper pole of the breast.