Varieties and atypical forms
This disease, depending on the health of the body and the type of carrier, can occur in several forms.
Ringworm occurs:
- Chronic - typical for women who have completed the process of puberty. In fact, it is a form of complication of superficial lichen hidden in childhood. The hormonal fluctuations that occur in the female body at the time of maturation undermine the immune system, which gives ringworm the opportunity to develop stronger.
- Superficial - white spots with a red border are almost harmless to humans, because the upper layer of the dermis is affected.
- Purulent - true to the name, diseased skin secretes pus. The parasite affects not only the surface of the dermis, but also the body as a whole, initially penetrating into the depths of the follicles, and then settling in the lymph nodes. This form is characterized by high temperature.
- Deep form - settles mainly on the skin of the legs, pseudomyceliums are formed in dense nodes at a depth of 3-4 cm.
- Plantar form - callus-like formations appear on the foot, they peel and hurt when walking.
- Nail - in appearance it is ordinary onychomycosis, with characteristic colored spots and separation of the nails.
- Abortive is the mildest form, manifested by pale pink rashes.
- Papular - the skin begins to actively loosen in places where centimeter-long bumps appear. One of the most unpleasant, from a cosmetic point of view, forms.
Pubertal boys do not suffer from the chronic form; in them the parasite dies on its own.
In addition to the form, the type of parasite that caused it plays an important role in choosing treatment tactics:
- Microsporia is a disease transmitted between people, of a zoonotic and anthropophilic type.
- Anthropophilic trichophytosis is an infectious disease with a fungal pathogen that is transmitted only between people.
- Zoonotic trichophytosis is similar to anthropophilic in nature, but is transmitted to humans from cattle, cats and other animals.
It is important to understand that ringworm is a common name that combines two different diseases (Microsporia and Trichophytosis) caused by different pathogens. The localization and clinical picture of both diseases are very similar, so historically they were considered a single disease, and later they were separated, thanks to in-depth medical research.
How does the disease progress and are there any consequences?
The incubation period for ringworm in humans lasts from 7-14 days to 6 weeks. The fungus eats the protein in the hair. Keratin is necessary for the growth and reproduction of fungus, as a result of which the hair shaft is destroyed. A colony of microorganisms grows, forming spots that can exceed several centimeters in size. The shape of the spots and appearance differ depending on the pathogen. The disease is characterized by itching, redness, and peeling.
At the first signs, you should contact for additional examination. If an infected person works in a school, there is a risk of infection among children and other adults.
The risk of baldness exists only in advanced cases, when lesions begin to cause wounds on the upper layers of the skin.
Chronic form of the disease
It is important to know how to treat ringworm on the head.
Since when the form is advanced, the disease becomes chronic and will be tormented by constant relapses. As a result, seborrhea develops and sebum production increases. In the deep form of the disease, a large painful plaque appears on the scalp, from which purulent fluid is released. In appearance it resembles a tumor formation. In men it can form in the mustache and beard.
If the affected hands are left without proper treatment, the disease causes the blurred contours of the spots to become pink to bluish in color. Peeling of the skin occurs.
Affected nails take on a gray, cloudy, dull color. The edges become jagged and crumble. The nail plate thickens.
Trichophytosis
Trichophytosis in humans manifests itself with certain symptoms, without treatment it leads to baldness, lowers the skin's immunity, making it vulnerable to other skin diseases. The causative agent is the fungus trichophytosis, which can affect any area of the skin. The disease develops in 3 stages:
- The incubation period lasts up to 2 weeks, on the 10th day you can see signs of the disease.
- In the acute form, inflamed spots of oval or round shape are formed, without clear boundaries. Hair breakage is observed at a distance of 1-2 mm from the root, and black dots form around it. At this stage, with a visual examination, a dermatologist can make an accurate diagnosis without additional examination.
- If the child is more than 12 years old, then trichophytosis goes away on its own. For adults, and especially for women, the disease is characterized by duration; there is also a risk of infection in children.
Baldness of the affected skin area.
Microsporia
The causative agent is fur-bearing animals. When a fungus gets on the skin, it provokes a disease characterized by the following stages:
- When in contact with a sick animal, it takes 7 days for the fungal disease to manifest; when in contact with an infected person, up to 6 weeks. Once the fungus has taken root in the body, it begins to camouflage itself, but when infected by an animal, it manifests itself faster.
- In the acute form, spots of a flaky structure form that cause itching. Then a bald spot appears, which can reach 5 cm in diameter.
- At an advanced stage, hair breaks off at a distance of 5 mm from the root, bald patches up to 2 cm in diameter appear. Fungal spores form cylindrical rings.
Without proper treatment, scars and bald patches form on the skin.
Drugs are used to treat ringworm in humans
Symptoms
Depending on the condition of the body, the depth of location of the fungal colony and which part of the body it has “chosen”, the clinical picture of the disease may vary, so the localization is as follows:
- torso,
- Feet,
- legs,
- hands,
- nails,
- groin and armpits,
- palms,
- face,
- skin under hair.
Therefore, the full name of the disease always sounds like this: Superficial ringworm of the trunk or Purulent ringworm of the scalp, etc.
In addition to general symptoms by type, there are also specific clinical signs that arise depending on the pathogen that caused the disease:
- Trichophytosis - the place of development of trichophytosis can be both smooth skin and areas under the hair. Initially, the lesions look like red-pink spots up to 2 cm in diameter. It all starts with one island, its surface slightly swollen, protruding above the level of the rest of the dermis. Even before a large number of lesions form, the first one becomes covered with flaky white scales that fall off when touched. The lesions systematically appear throughout the body, but at the same time they are located separately and do not merge into the general pathology, as with tinea versicolor. At the next stage, one of the colonies becomes the main one - its size is significantly larger than the other foci, and its edges look like a torn flower. At the last stage of development of the disease, if left untreated, the lesions turn into rings with a dense crust in the middle, and the hair breaks off completely in these areas. The favorite places for trichophytosis are the torso, neck, face and forearms, but sometimes there are exceptions and the parasite breeds on the scalp.
- Infiltrative-suppurative trichophytosis - this subspecies of the fungus is classified as a separate group, because the pathogen is zoophilic. This disease is most widespread in rural areas; it is sometimes called an occupational disease of a veterinarian-animal breeder. Unlike its counterpart described above, the inflammatory process begins immediately after infection and develops extremely quickly, up to suppuration in the affected areas. The bestial pathogen immediately affects all areas of the epidermis, simultaneously developing on smooth skin and areas of hair growth on the head, while it is very fond of mustaches, beards, and eyebrows. Having reached the stage of suppuration, the lesions acquire a blue-purple color, their surface is covered with tubercles that form scabs, erosions and scales. When pressing on the skin, pus is clearly released from the mouths of the follicles; under such conditions, the hair falls out along with the follicles. A kind of “honeycomb” forms on the head, which softens only with proper treatment.
- Microsporia - during the first 4-7 days of infection, the parasite remains in the incubation period, so it does not manifest itself in any way. Afterwards, the clinic appears depending on the location of the development of the lesion: Scalp - a round lesion with a diameter of 3 cm suddenly appears. It is covered with gray scales, after which the hair in the affected area breaks off (a fracture occurs at a height of 5 mm). In subsequent stages, the lesion and remaining hair are covered with a noticeable white coating.
- Smooth skin - spots have a diameter of up to 2 cm and are light pink in color. When the colony stabilizes, it will begin to grow, with the center of the circles becoming lighter and the border highlighted by papules. If the fungus is not treated, then double, triple, etc. will begin to appear inside the lesion. inner circles.
A person who has had infiltrative-suppurative trichophytosis, in addition to scars for life, acquires complete immunity to the pathogen, so relapse is impossible.
How do you understand that you have this particular disease?
Ringworm in humans manifests itself with characteristic symptoms. To diagnose, it is necessary to conduct an external examination and scrape the affected skin. The hairs are also examined, as ringworm fungi may be present there. Using a special lamp, when illuminated, the affected hairs emit an emerald green color.
The symptoms of ringworm may be similar to those of other diseases, so it is necessary to accurately determine it, since the recovery and health of other people depends on it. In this case, the disease can affect any part of the body:
- Skin of hands, feet;
- Feet;
- Toe and hand nails;
- Armpits, inguinal folds;
- Scalp;
- Facial skin;
- Palms of hands.
Depending on the location of the disease, the signs of ringworm may vary.
The initial stage of ringworm on the head is manifested by symptoms:
- The appearance of round lesions, hair thinning, then the hairs break off;
- Peeling skin, gray-white scales, similar to dandruff;
- Redness of the skin and the appearance of blisters, followed by a yellowish crust;
- The size of the affected area can reach 3-10 cm;
- Itching.
The first signs of ringworm on the skin are similar to pityriasis rosea. If this factor is not taken into account, then incorrect treatment may be provided. Pityriasis rosea occurs only on the face, hands, and feet, which is the main difference.
Photo of ringworm in humans:
Symptoms of ringworm are characterized by spots with clear contours of bright color. In the center the skin is light in color with gray scales. The lesion may increase in diameter and cause itching.
Photo of ringworm: what it looks like
An animal suffering from ringworm suffers greatly, but you need to worry not only about its health, but also about your own. If your pet has minimal prerequisites for the disease, urgently take him to the hospital, and after that, immediately go for an examination to a dermatologist with the whole family.
Content may be difficult to view
A classic example of developing microsporia in the scalp area. The photo shows a characteristic gray coating that densely covers the affected area.
The stage of formation of the main colony in trichophytosis. In the photo you can see how much larger the main hearth is than its ordinary counterparts.
A rare form of ringworm that affects the nails. This happens really rarely, this onychomycosis develops very quickly, and the course of treatment will be 6-12 months, which makes it very difficult to follow all the doctor’s recommendations and makes this form the most difficult to remove from all varieties of ringworm.
Prevention of the disease
Prevention of ringworm for humans consists of maintaining hygiene and avoiding contact with stray animals. This is especially true for children. It is important to ensure that your child does not play with stray animals.
If baldness is detected on an animal, while the whiskers have shortened, then this is a clear sign of disease. The animal must be taken to a veterinarian. After this, you need to carefully examine your skin and hair for 2 months.
Interesting! A child under 12 years of age has not developed immunity, nor has an opportunistic microflora formed.
Diagnostics
The accurate diagnostic technique consists of two main stages and several additional ones.
Main stages:
- Examination - the doctor visually examines the lesions, collects anamnesis and biological material (scraping, hair roots).
- Bacterioscopic examination is a substantive study of the remains of the pathogen and its reaction to inoculation in a nutrient medium.
Auxiliary methods:
- Voodoo lamp - used for suspected microsporia; the second name for this method is fluorescent diagnostics.
- Differentiation - it is very important for doctors to distinguish ringworm from alopecia, favus, eczema or psoriasis, and in the case of deep ringworm from ostiofolliculitis and cellulitis.
Diagnosis of trichophytosis
If symptoms characteristic of the disease appear, immediate contact with a dermatologist is required to prevent the spread of the fungal infection to other people.
First, a visual examination of the patient, lesions on the head and skin is carried out. To establish an accurate diagnosis, the doctor takes a scraping from the inflammatory elements to examine the material in the laboratory. This is necessary to identify the causative agent of the disease in order to know for sure how to fight it.
Another type of diagnostics is the use of a special fluorescent lamp. Lesions affected by trichophytons usually glow green.
Methodology for treating ringworm
Treatment for ringworm is aimed at exterminating the fungus that led to dermatomycosis (sometimes to onychomycosis). Self-medication in this case is very dangerous, because it is impossible to classify the parasitic fungus without laboratory tests, and improper treatment can, at a minimum, disrupt the antagonistic balance and stimulate the growth of the disease. Typically, a dermatologist chooses complex therapy, consisting of both external agents and oral medications. The duration of treatment and dosage of medications used depends on: the type of parasite, the form of the disease and the stage at which the patient consulted a dermatologist.
The specialist doctor for ringworm is a mycologist, but it is extremely difficult to find one, especially in small towns. Therefore, it is better to simply go to a dermatologist working in a skin and venereal disease clinic - such a solution will provide you with high-quality treatment and eliminate the need to look for a rare and expensive specialist.
Ointments
This form factor differs from other external products in that it remains on the surface of the skin for a long time, due to which the active substances are better absorbed. The treatment regimen with ointments for ringworm is always combined with iodine. Typically, the ointment involves application in the evening (before bedtime), and in the morning the lesions are lubricated with iodine.
Recommended ointments:
- Ciclopirox,
- Salicylic acid,
- Mycosporus,
- Lamisil,
- Sernaya,
- Clotrimazole,
- Sulfur-tar,
- Bifonazole.
Before applying external products, it is advisable to take care of cleansing the skin. This can be done with potassium permanganate or furatsilin.
In cases where conventional ointments have little effect on the fungus, the doctor may prescribe hormonal external agents: Travocort or Mycozolon.
Gels and solutions
This treatment option is used when there is a thick stratum corneum caused by the parasite, as well as when it comes to treating the scalp, because they do not stain the hair.
The most popular:
- Mikogel-KMP,
- exifin,
- Yoddicerin,
- Vokadin,
- Nitrofungin.
Pills
This technique is used exclusively in cases where diffuse rashes appear on the skin or there is deep damage to the follicles and internal organs of the patient. Oral medications not only fight the parasite itself, some of them accumulate in the body and prevent relapses.
The most popular tablets:
- Griseofulvin,
- Orungal,
- Lamisil.
All complex drugs have side effects, so using them without a doctor’s prescription is strictly prohibited.
Shampoos
These cosmetics for ringworm are used to achieve a certain effect depending on the type of disease and its stage, as follows:
- Sulsen - disrupts the antagonistic balance in a direction unfavorable for the fungus;
- Nizoral, Dermazol, Ketoconazole - act directly on the parasite itself;
- Tar shampoo - used for drying the scalp and general disinfection, in order to avoid associated diseases.
Diet
To prevent your immune system from suffering from an unbalanced diet, if you have ringworm, you need to follow general recommendations: control fats and carbohydrates, don’t forget about fiber, eat fresh foods, and be sure to take the vitamins your body needs.
Forbidden foods are of much greater interest, because their consumption can greatly contribute to the disease:
- alcohol,
- sweets,
- nutritional supplements,
- spicy dishes,
- mushrooms,
- beans,
- lard and fat.
At the same time, you can drink tea, coffee and cocoa, within reasonable limits.
ethnoscience
The thing you definitely shouldn’t do when you have ringworm is treat it yourself. It is almost impossible to determine the pathogen and form at home, so traditional medicine is used as an addition to medical treatment.
Popular among the people are:
- Apple cider vinegar - wipe the affected areas 5-7 times a day with undiluted 5% apple cider vinegar. If there is severe burning and additional irritation, treatment is stopped.
- Olive Oil and Sulfur – Add olive oil slowly to the hot sulfur. The resulting thick paste is used to smear the areas of lichen.
- Herbal mixture - celandine, horsetail, tripartite string are mixed in proportions 2:1:4, after which 2 tbsp. The resulting mixture is steamed in a glass of boiling water for 1 hour. The tincture is rubbed into the infected skin after taking a shower.
- Cabbage compresses with sour cream - a fresh, clean cabbage leaf is applied to the lichen lesion for an hour, after which the area is smeared with sour cream and secured with a bandage.
- Ointment from burdock root, hop cones and calendula - the ingredients are mixed in a ratio of 2:2:1 (in grams) and a strong decoction is boiled from them, after which the resulting liquid is mixed with petroleum jelly in a ratio of 1:2. The ointment is applied twice a day to areas with lichen and is not washed off.
Recommendations
In addition to food preferences, for a speedy recovery, eliminating the possibility of infecting others and preventing relapses, the patient needs:
- Wear daily replaced knitted underwear and the same cap.
- Wash clothes separately from others, boil them and iron them at high temperatures.
- Follow the doctor's recommendations when taking a shower: cover the necessary areas with cling film, use special shampoos.
- Try not to touch things that are difficult to clean - pillows, carpets, etc. Change your bed linen every day, and buy thick pillowcases for pillows.
- Carry out wet cleaning of the house daily.
- Separate your own hygiene products from the same products that the rest of the family uses.
How to quickly cure ringworm in humans
When treating ringworm in humans, the basis of therapy is the fight against the fungus that causes dermatomycosis. Treatment is prescribed only by a dermatologist; it combines local treatment with ointments for lichen - antifungal creams, sprays, shampoos with oral antifungal drugs.
- Ringworm of smooth skin responds better to treatment with Terbinafine and tolnaftate.
- For local treatment, the doctor may recommend various ointments, creams, shampoos containing Clotrimazole, Ketoconazole, Mycoseptin, Terbinafine, Mycoconazole. (Local antifungal agents - creams, sprays, gels).
- To treat lichen in the morning, a 5% iodine solution is usually used. In the evening, as a rule, sulfur-salicylic or sulfur-tar ointment is prescribed; treatment with pure salicylic acid 3% is also possible.
- A doctor can write out a prescription for the production of Vidal's milk in the prescription department of a pharmacy - alcohol, camphor, salicylic acid, sulfur lotion, boric acid, glycerin. Or Lassar pastes - petroleum jelly, starch, salicylic acid, zinc oxide.
For systemic treatment of dermatomycosis, Griseofulvin is used; it is a natural antimycotic that has a narrow spectrum of action, namely, it is active against dermatomycete fungi, Trichophyton, Microsporum, Epydermophyton, Achorionum.
- Treatment of ringworm of both the skin and hair is necessarily accompanied by oral administration of griseofulvin. It should be taken for 15-25 days, and a bacterioscopic scraping should be taken once a week to detect fungus. As soon as the fungus is not detected, the intake of griseofulvin is continued every other day, at the same dose that the doctor calculated, for another 14 days, so that there is no relapse of the disease.
- If the feet are affected by the fungus, it is recommended that they be treated with Ketoconazole or Clotrimazole orally, and selenium sulfide applied externally.
For the treatment of chronic ringworm, in addition to antifungal agents, both local and oral (Griseofulvin), vitamin therapy, immunomodulators, and drugs that strengthen blood vessels and improve microcirculation are also indicated.
It is very important to observe hygiene measures, since fungal spores disperse around the patient, and after 1-3 months a relapse of the disease may occur, and the risk of contracting ringworm to other relatives is very high.
Remember the following recommendations from experts:
- the underwear of a patient with ringworm should be washed separately, and before washing it should be soaked in a disinfectant solution or boiled;
- All linen and clothes of the patient must be ironed after washing;
- every day in the patient’s room and in general in all places where he happens to be, it is necessary to carry out wet cleaning with any disinfectant;
- absolutely all items used by the patient must be treated with a disinfectant every day;
- During the illness, carpets, soft toys, textiles and all things that are difficult to clean are removed from the room where the patient is.
Can ringworm go away without treatment?
The possibility of ridding the body of ringworm on its own exists, but it is negligible. Science knows of several cases where the disease resolved without any medical intervention, however, these are isolated phenomena. Most often, the infection, having caused inflammation once, begins to spread further. If the disease developed in childhood and was not treated, it will persist until adulthood.
What should I do if I get ringworm during pregnancy?
Do not panic if the infection develops during gestation, since these mycotic organisms are not able to have a pronounced effect on either the child or the woman. If infected, you should consult a doctor and undergo the treatment recommended by him. During pregnancy, oral medications are not prescribed to get rid of the infection; it will be enough to use ointments prescribed by the doctor.
Prevention
In addition to general hygiene measures, there are specific rules of behavior when a patient infected with ringworm appears in the house:
- daily external examination of all family members;
- constant disinfection of common areas;
- daily shower;
- wash your hands with tar soap after any visit to public places;
- regular examination of pets;
- contacting a specialist should occur no later than 24 hours after detection of suspicious symptoms.
Diagnosis of microsporia
Diagnosis of microsporia is based on the clinical picture of the disease, epidemic history (contact with cats, dogs or sick people), microscopic and cultural data, and the presence of an emerald glow under a Wood's lamp.
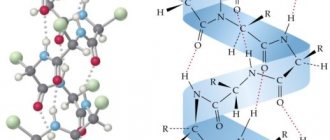
Microscopic examination
Microscopic examination reveals the presence of fungal mycelium and spores. It is impossible to differentiate microsporia and trichophytosis by microscopy. Identification of pathogens is carried out using a culture method followed by microscopy.
The material for microscopy is the patient's scales and hair taken from the peripheral zone of the lesion. Hair breaks off 3 weeks after the onset of the disease.
With microsporia, under a microscope, the affected hair has a characteristic appearance:
- It is surrounded by numerous round spores, tightly adjacent to each other in chains in the form of a mosaic.
- The peripheral internal part is filled with septate mycelium.
- At the end of the hair shaft, a fringe consisting of mycelium threads is sometimes visible.
- In the scales taken for research, branching mycelium with clearly defined sparse partitions can be found.
- In the affected nails, fungal elements are similar to those in the scales.
Rice. 23. Microscopy of the affected hair with ringworm.
Rice. 24. In the photo on the left is a hair affected by Microsporum canis, on the right - Microsporum
Rice. 25. Microscopy of the affected hair with trichophytosis. Pathogen spores envelop the hair like a muff (photo on the left). The inside is filled with spores (photo on the right).
Diagnosis of ringworm using a Wood's fluorescent lamp
At the base of the hair, 10 - 12 days from the moment of infection, an emerald-colored glow appears in the rays of a Wood's lamp. The study should be repeated after 3 days.
Wood's lamp is a quartz lamp. Ultraviolet radiation passes through glass saturated with potassium salts. The examination is carried out in the dark. Hair should be washed with soap before the examination. This technique is widely used by medical professionals to identify sick people and animals.
Rice. 26. The emerald glow when using a Wood's lamp is characteristic only of microsporia.
Rice. 27. Wood's lamp is used to identify ringworm and monitor the effectiveness of treatment. An emerald-colored glow in a person (photo on the left) and an animal (photo on the right).
Differential diagnosis of ringworm
Differential diagnosis of ringworm is carried out with seborrheic dermatitis, a limited form of neurodermatitis, psoriasis, alopecia areata, discoid lupus erythematosus; in the suppurative form of microsporia - with trichophytosis, boil, carbuncle, favus.
Possible complications and consequences
The most terrible complication after ringworm is that the hair may not grow back, and the scars from the disease may remain for life. This problem especially often occurs if treatment was started late or the doctor’s recommendations were violated. There is no danger to health, but the aesthetic appearance of a person who has received such consequences leaves much to be desired.
South Korean plastic surgery can completely solve the problem of unregenerated hair and scars, but it is quite expensive.
Questions for a dermatologist
During a ringworm illness, a person is contagious, so contact can infect others.
How long does it take to treat ringworm?
No one can say for sure how long it takes to treat ringworm. It all depends on the form and stage of the disease, on impeccable adherence to the treatment regimen, which usually lasts up to 6 weeks.
When the hairline is restored, the fungi begin to feed on keratin again and characteristic spots appear. Therefore, after recovery, the patient is under observation by a dermatologist for 3 months. During this period, a person undergoes tests 3 times to detect a relapse of the disease.
Will hair grow at the site of the plaque?
After treatment, hair grows back. But on the affected area of the scalp with advanced disease, hair will no longer grow. Therefore, it is important not to let the disease progress and to start therapy on time.
Contagiousness
The main way to become infected is through household contact, that is, a person needs to come into contact with a sick person (animal or person) or things he has touched. Moreover, both trichophytosis and microsporia are transmitted in this way; accordingly, active children under the age of 15 are most at risk; they easily come into contact with animals and other children. Ringworm is a persistent, highly contagious disease; it can be caught even in a hairdresser, if the hairdresser does not properly care for the tool. Sometimes healthy people can also be carriers; the parasite simply sleeps on their integument without developing due to the high immunity of the carrier.
The following have a particularly beneficial effect on the possibility of infection:
- maceration - softening of the integument during prolonged bathing;
- violation of the mechanical integrity of the external integument in any manifestation;
- diseases that weaken the immune system;
- stress, overwork, sleep disturbances.
Pityriasis rosea on the head
In addition to ringworm, other types of infectious lesions may appear on the head and body of a person. One of them is considered to be pityriasis rosea, which occurs in most cases against the background of reduced immunity. This disease does not require special treatment, since the immune system must cope with the infection on its own. The duration of the disease depends on the size of the area of infection.
The reasons why a person develops pityriasis rosea have not been precisely identified. But there is an assumption about the influence of the following factors on the development of a dermatological disease:
- viral infection;
- allergies to medications;
- seasonal factor;
- fungal infection;
- metabolic failures;
- ailments of the gastrointestinal tract;
- severe stress.
ringworm on the head in the photo
Symptoms of pityriasis rosea are very similar to the signs of other epidermal lesions. More often it appears on the skin of the body, but it can also occur on the head. Just as with ringworm caused by trichophytons, roseola flaking spots have clear and brighter outlines compared to the middle, rising above the epidermis. They differ in sensations of itching and burning.
The symptoms of the disease on the scalp are exactly the same as on the smooth skin of the body. The development of roseola may be accompanied by signs of viral damage to the body, similar to the symptoms of ordinary flu. We are talking about general malaise, headache and joint pain, runny nose, sore throat, etc.
Children suffer from this disease in the same way as adult patients.
After diagnostic procedures, the dermatologist may recommend the use of the following methods to speed up recovery:
- if intense itching sensations bother you, then taking antihistamines is advisable;
- it is necessary to exclude from the diet foods that can cause allergies;
- It is important to take vitamins to strengthen your immune system;
- prevent moisture from entering the affected areas of the skin;
- you cannot sunbathe in the sun or visit a solarium;
- it is required to use ointments and creams for local treatment of lichen;
- in some cases antibiotics are prescribed.
Just like ringworm, roseola scaly is a pilaris, the pathogens of which penetrate the hair follicle, contributing to its fragility and destruction. Due to fragile immunity, lichen pilaris in most cases is diagnosed in children who have not reached puberty.
Features in children
There are several features characteristic only of this group of patients:
- at a young age, ringworm, regardless of its form and pathogen, can settle on any part of the body, the scalp is especially often affected;
- Most often, suppurative and infiltrative forms develop in children;
- Regardless of the type, ringworm in children causes inflammation of the lymphatic system;
- Very often, ringworm in a child is accompanied by fever.
Features of treatment for children
Ringworm occurs in children much more often than in adults and has its own characteristics, on which treatment tactics depend. Children are more susceptible to allergic reactions; they are more likely to experience multiple lesions and infections of skin areas.
When prescribing therapy, it is important to prevent it from becoming chronic (insufficient doses and course duration), but also not to cause adverse reactions and complications from taking rather toxic antifungal drugs. The principles boil down to the following:
- mandatory prescription of antihistamines. The lesions cause severe itching, so young patients scratch the primary lesion;
- a combination of specific local drugs and anti-inflammatory ointments. Children, scratching elements of lichen, cause a secondary bacterial infection;
- preference is given to local antifungal agents. The decision on systemic treatment is made only by the doctor;
- children must be strictly isolated from their peers, otherwise ringworm will quickly spread in the children's group;
- means are always prescribed to strengthen the immune system. The diet is enriched with proteins and vitamins; the child should not worry too much about his diagnosis (this often happens in adolescence); sometimes light sedatives are required.
In boys, ringworm can sometimes heal on its own. In such cases, it is important to check whether the cure is complete, otherwise the process will transform into a chronic form.
Pregnancy and lactation
The fetus cannot become infected with ringworm during gestation, but the disease brings significant discomfort to the mother in labor.
There are several features for treatment during this period:
- It is prohibited to be treated with complex and hormonal drugs, even if they are external agents;
- underwear should be changed twice a day to avoid vaginal infections;
- Taking your child to bed with you is strictly prohibited;
- When feeding, you should never let it come into contact with the affected areas of the body; cover them with a sheet or oilcloth.
It is also impossible to simply ignore the process during this period: firstly, by the time the child is born, the whole house will be infected, and secondly, the disease is fraught with a chronic form and corresponding consequences. The main thing is not to self-medicate and contact the appropriate doctor.
Can shingles be transmitted to another person?
One of the ways ringworm is transmitted is through stray cats and dogs, especially through puppies and kittens. Elements of infected fur fall on the skin, and infection occurs.
Through direct contact or through personal objects (loofah, hat, comb), a healthy person can become infected from an infected person.
During the period when ringworm begins, the disease can be detected by examination with a fluorescent lamp. The hairline emits a characteristic greenish tint. As soon as the first signs are detected, you need to contact a dermatologist who will prescribe effective remedies to cure ringworm.
It is necessary to treat lichen in a person, for how long, how long is necessary to reduce the blisters and cleanse the skin of the crust. During treatment, infection of other people does not occur.
Interesting! When spores fall on the soil, the fungus continues to live for up to 3 months, after which they lose activity.
Signs and clinical forms
The symptoms of trichophytosis are quite recognizable. The main one is the appearance of reddish spots on the body, sharply demarcated from the surface of healthy skin. The spots may be round or shapeless. Color varies from pale pink to red-violet. The surface can be smooth or rough. Often, a slight pityriasis-like peeling forms in the center of the spot, which disappears closer to the edges. The boundaries of the spot can be blurred or pronounced. In the second case, blisters or purulent hemorrhagic crusts are clearly visible.
The mycelium growth zone can be in the same plane as the skin, 2-3 mm above it. When the deep layers of the dermis are involved in the inflammatory process, a spherical “bump” appears at the site of the spot. It protrudes over healthy skin. There may be discharge on the surface:
- bloody;
- purulent;
- hemorrhagic.
The lump consists of an inflammatory infiltrate. As the disease progresses, pus accumulates in the skin.
Trichophytosis is characterized by a particularly recognizable symptom - the presence of “stumps” over the entire surface of fungal spots. “Stumps” are broken hairs that have been infected by a fungus. The appendages break off 2-3 mm from the skin, and their remains are clearly visible to the naked eye. Sometimes the “stumps” become covered with a grayish coating.
The second scenario is lysis of the hair sheath by the fungus and destruction of the hair directly near the hair follicle. In this case, there are no stumps, but black dots are visible on the skin - fungus-filled passages that remain from lost hair.
Lichen planus
Other names of the pathology: Lassuer-Little syndrome - name. in honor of the early explorers, lichen cicatricial and follicular erythematosus. The disease rarely affects human skin, and it is not the epithelium that is affected, but the hair follicles. The reason for its occurrence is still controversial. According to scientists, the pathology is hereditary in nature, can be transmitted from either parent, and develops when there is a lack of vitamin A in the body (necessary for the health of the immune system).
Clinical picture
The symptoms that precede the appearance of lichen follicularis on the scalp first manifest themselves as a feeling of itching, then the appearance of a pointed nodular rash and hair loss. In this case, papular rashes can form not only on the head, but also on other parts of the body (torso, limbs - on the folds).
Note! With lichen follicularis, the skin at the site of its appearance does not become inflamed. The affected surface is rough.
Bald spots form in the temple area, on the back of the head and crown. They have a round shape, and with medical inactivity they begin to slowly increase. Merging, small bald spots form large areas of baldness on the patient’s head (they can affect the entire scalp).
Skin affected by lichen follicularis differs from healthy areas in having a shiny and noticeably stretched surface. In most cases, the diseased skin has a color close to natural, but may change to blue-pink. Serous crusts form at the site of scratching.
Note. Lichen planus is difficult to cure, because often after an improvement in the patient’s clinical condition, an exacerbation of the disease follows.
Diagnosis of the disease
Lichen follicularis cannot be diagnosed through general and biochemical analysis (blood and urine tests). The external symptoms of this form of skin disease do not always appear the same. Typically, upon examination, patients present with a lichenoid rash (shiny, flat nodules) and hair loss.
When conducting a histological examination in pathological foci, the following is revealed:
- Dystrophic change in the basal layer of the skin (adjacent to the dermis).
- The presence of infiltrate in the spinous layer of the epidermis (located above the basal layer).
- Unevenness of the granular layer of the epidermis.
In order to clarify the diagnosis, a differential diagnosis is carried out, which makes it possible to separate lichen planus from monilethrix (pathology causes hair atrophy throughout the body) and keratosis pilaris (horny plugs form at the mouths of the follicles).
Features of treatment
Doctors have still not been able to formulate an effective treatment regimen for lichen pilaris.
To treat this form of the disease, patients are prescribed the following drugs:
- “Plaquenil”, “Delagil” are anti-malarial drugs that have an anti-inflammatory, antiprotozoal (activity against protozoan parasites: amoebas, lamblia, trichomonas) and a strong immunosuppressive effect on the body (suppresses the excessive activity of the immune system when it begins to attack the body’s cells, mistaking them for alien).
- Vitamin A or “Aevit” - participates in the formation of the structure of hair and nails, fat accumulation, normalizes metabolism, strengthens the immune system.
- Local preparations with corticosteroids (Prednisolone, Tetracycline, Hydrocortisone) have an immunosuppressive (depresses the immune system) and anti-inflammatory effect.
In order to restore the natural shade of damaged skin, patients may be prescribed photochemotherapy.
Also, lichen can be treated with ointments, which are usually not used to treat lichen on the head, but if you have lichen on the body, then this is the most effective treatment with these drugs.
Treatment
To make a diagnosis and prescribe adequate therapy, a laboratory examination of skin flakes or nail plates and isolation of a fungal culture are necessary.
Differential diagnosis of trichophytosis is carried out with:
- microsporia;
- rubrophytia;
- favus;
- seborrheic eczema;
- pityriasis rosea;
- athlete's foot inguinal.
The infectious-suppurative form is differentiated from:
- microsporia;
- pyoderma. Here you can read in detail about pyoderma in children.
- psoriasis.
Treatment is a combination of drugs for general and local use. Medications should only be taken as prescribed by a specialist. For single lesions located on the surface of the ugly skin, only external medications can be used.
Systemic drugs
Antifungal drugs are used orally, such as:
- griseofulvin;
- levorin;
- nystatin in an individual dose.
To increase the activity of the immune system, general strengthening drugs are prescribed:
- adaptogens (ginseng, eleutherococcus, lemongrass, roseola rosea, ginger);
- vitamins A and E (which are keratoplastics).
The most preferred antifungal drugs are:
- Orungal (based on itraconazole) and exifin (based on terbinafine). The presented medications are most effective, which allows them to be taken for a minimum period of time 1-2 times a day. Moreover, these products are low-toxic, which means they can be used in childhood.
- Griseofulvin. It is not inferior in effectiveness to the analogues presented above, has a much lower cost, but the number of daily doses increases up to 3 times and the course duration increases up to 6 weeks. In addition, griseofulvin has an inhibitory effect on the immune system and can interfere with the absorption of B vitamins, so its use must be combined with vitamin therapy and immunocorrective drugs (Immudon, Thymalin, Taktivin).
Local treatment
Hair needs to be shaved. This recommendation applies to hair on the head, eyebrows, mustache, beard, and vellus hair located on other surfaces of the body. If the eyelid is affected, it is necessary to manually remove the eyelashes (using tweezers).
Applications with 3% salicylic, tar ointment, Wilkinson's ointment or 2% are applied to the affected area.
alcohol solution of iodine. Shampoos containing antifungal agents (mycoseptin, fluconazole, ketoconazole) are very effective.
There is a huge selection of different antifungal ointments:
- funginal (3 times a day for 20 days);
- mycogel (2 times a day for 20 days);
- exoderil (2 times within 14 days);
- Lamisil (1 time for 7 days);
- exifin (1-2 times for 7 days).
Personal hygiene
Hygiene is one of the most important steps in both the prevention and elimination of ringworm.
Necessary measures to be taken after contact with an infected person or animal:
- treat hands and contacted areas of skin with soap and antiseptic or other antiseptic agents (chlorhexyline, miramistin);
- apply a cream with a fungicidal or fungistatic effect (amiclon, afitin, binafine, canison and others);
- in case of possible damage to the scalp, it is necessary to wash it with shampoo with an antifungal effect (keto-plus, mycozoral, nizoral);
- for preventive purposes, it is very convenient to use fungicidal sprays, which can be used to treat not only your own skin surface, but also other surfaces, to prevent contact and household transmission of infection (Lamitel, Lamisil, Canesten);
- exclude mutual use of objects (combs, clothes, etc.).
Reasons for appearance
Ringworm develops under the influence of a pathogenic fungus of the genus Microsporum, which forms a large number of microscopic spores. The fungus affects not only the skin, but also the scalp and nails.
Microsporia in animals and its causative agent, a fungus of the genus Microsporum under a microscope
Dermatophytosis is transmitted in the following ways:
- upon contact with an infected person;
- when using things and personal items of an infected person;
- when staying in the same room with an infected person for a long time.
Risk factors are:
- frequent stress and anxiety;
- violation of the integrity of the skin;
- working with soil without using protective gloves;
- increased humidity, at which the skin softens;
- lack of vitamins in the body;
- dysfunction of the sebaceous glands;
- reduced immunity.
If there are no predisposing factors, then the chances of infection are reduced: the fungal cells are destroyed by the immune system.
The incubation period of this fungal disease is 1.5-2 months.
Forecast
Modern treatment methods and medications can make the prognosis favorable. Subject to proper treatment and following all the recommendations of the attending physician, after getting rid of ringworm, the symptoms of the disease disappear, and the hairline is completely restored.
Microsporia is considered a fairly common disease among young children and adults who do not follow hygiene rules and often come into contact with animals . Preventive measures and careful attention to your own health will help you avoid infection.
Mechanism of infection
Trichophytosis can be “caught” from a person or animal. In the first case, the infection is considered anthropophilic, and in the second – zoophilic. The carrier does not always show signs of the disease.
Children of primary and school age are more susceptible to infection. The percentage of detection of trichophytosis among the adult population is equal for women and men, working people and the elderly.
The disease provokes the contact of fungal spores with areas of exposed skin or hair. The “sleeping” fungus begins to germinate and forms mycelium in the surface structures of the epidermis. The infection affects body hair (on hairy areas of the skin, vellus hair on smooth skin). Hair becomes thinner, dull, brittle and breaks off. In the dermis, a fungal infection provokes inflammation, and sometimes the formation of ulcers and abscesses. Without appropriate treatment, the fungus may spread to large areas of the body, skin scarring, and permanent baldness.
Anthropophilic infection is most often transmitted through household contacts, sharing combs, towels, and household appliances. When infected within a family, the infection is usually transmitted to family members from the mother. Relatives become infected through close physical contact (hugs, touching).
Zoophilic trichophytosis is spread by homeless animals. Even with hand washing and good hygiene, the risk of infection remains. It is especially high for those people who work in places where animals are concentrated (farm, veterinary clinic, shelter, charitable organizations), with regular contact with them.
The likelihood of infection for a person increases with decreased immunity. Infectious diseases, exhaustion, vitamin deficiency are predisposing factors for trichophytosis.
Folk recipes
There are also traditional methods of treating ringworm. The most effective and common means are:
- smoke treatment. It is recommended to take a clove of garlic and a little tar, mix and set it on fire. When smoke starts to appear, hold the affected area over it. The duration of the procedure is 5-7 minutes;
- medicinal baths. Pour 100 g of celandine herb into 4 liters of cold water. Bring the broth to a boil, remove from heat, cool and leave for an hour. Strain the resulting liquid, pour it into a bath of water at a temperature of 45 degrees and remain in this composition for 10 minutes;
- Apple vinegar. Moisten a cotton swab with natural vinegar and wipe the affected areas up to 6 times a day. It is also useful to apply compresses and leave them for 10 minutes;
- chamomile infusion for the treatment of lichen on the head. Add half a tablespoon of chamomile petals and a glass of boiling water, let it brew for 20 minutes. Rub the infusion into the scalp 30 minutes before washing your hair;
- cranberry juice. Squeeze juice from a handful of fresh berries. Apply the resulting liquid to the affected areas and do not wash off until completely dry;
- cabbage leaf Mash the cabbage leaf using a wooden mortar and squeeze out the juice. Apply it to the affected area and leave for an hour. Then treat the affected area with rich sour cream and wrap it with a bandage.
Therapeutic baths with a decoction of celandine will help you get rid of lichen faster.
To speed up the treatment process, you must also follow a therapeutic diet. Those who suffer from ringworm should eat more dairy products, nuts, sorrel, cereal side dishes, grapes, and carrots.
If you have a fungal disease, you should avoid hot sauces, a variety of spices, fatty foods, processed foods, and foods with flavors and flavor enhancers. It is also necessary to stop drinking alcohol.
Prevention methods
To prevent infection with a fungus of the genus Microsporum, the following rules should be followed:
- observe the rules of personal hygiene;
- use tar soap, which has an antifungal effect;
- carry out wet cleaning of the premises daily using disinfectants;
- When bathing, use a soft washcloth that does not violate the integrity of the skin;
- carry out heat treatment of underwear and bed linen, clothing;
- wash your hair with antifungal shampoo.
If there is contact with an infected animal or person, you must immediately contact a specialist and undergo the necessary tests.
Drug therapy
Conservative treatment involves the use of targeted medications, that is, various gels and ointments, as well as oral medications that act on the causative agents of the disease from the inside.
When treating ringworm, the following topical medications are recommended:
- Sulfuric ointment. The drug contains tar. It is recommended to apply it before bed, locally, to the affected areas of the skin.
- Exoderil. The ointment is quickly absorbed and concentrated in the quantities necessary to suppress the activity of pathogenic fungi. It should be applied to problem areas once a day.
- Mycoseptin. The product is used to eliminate stains that form on the skin. The affected areas should be lubricated twice a day.
- Nitrofungin. This topical drug is available in the form of a solution. It can be used as a stand-alone medicine or as part of complex therapy with ointments and creams. It is recommended to use it several times a day.
- Lamisil. The product has an antifungal effect. It is applied in a thin layer to the affected areas in the morning and evening.
If the disease is advanced, oral medications are added to targeted drugs. For ringworm, the patient can be cured with the help of tablets such as:
- Griseofulvin. The drug has an antifungal effect. The substance affects the intracellular processes of pathogens, blocking the possibility of their further growth and reproduction. The dose is calculated based on the patient's weight. The standard dose is 2 tablets 4 times a day. It is recommended to take Griseofulvin with oil.
- Orungal. The drug destroys the shell of the pathogen. The course of treatment is about 15 days.
- Terbinafine. The peculiarity of the tablets is that they are well tolerated by patients. It is recommended to take one tablet before bedtime. They can be taken by pregnant women and children as prescribed by a doctor.