When a person develops a myocardial infarction, blood flow in one or more coronary vessels is disrupted. This leads to an imbalance between the need of myocardiocytes for oxygen and its supply. Changes in metabolism due to lack of nutrients aggravate the condition of the affected tissue. As a result, cardiac muscle cells begin to necrotize and die. In place of the dead tissue, a scar forms. In this article I want to talk about the mechanism and possible consequences of such a “replacement”.
Development mechanism
At the time of the development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Classification
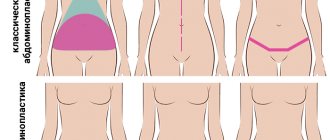
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
Rest and sleep
The postoperative period after heart surgery may be accompanied by problems with sleep, but after 3 months the sleep pattern should return.
If pain bothers you, you will need to take medications about half an hour before bedtime. You also need to arrange a comfortable bed, perhaps listening to relaxing music before bed will help the patient.
In the evening, it is recommended to avoid caffeine, including chocolate, coffee and tea.
Call your doctor if your sleep begins to affect your mood or behavior.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can be observed from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
How dangerous is this?
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
What causes scarring on the heart muscle?
What is a heart scar? In fact, it is connective tissue that fills the space created as a result of damage to a certain area of the heart muscle. This happens with an inflammatory disease or myocardial infarction, which is caused by various factors. The appearance of numerous notches on the heart can occur due to progressive vascular atherosclerosis.
The appearance of scars is caused by the death of heart cells as a result of blocking the access of oxygen-enriched blood to them. A common cause of heart scars is thrombosis. If a person has a prolonged vascular spasm, this will lead to partial necrosis of the organ. Other diseases that cause scarring of the heart include:
- Cardiac form of rheumatism. With this type of disease, inflammation of the myocardium and cardiac membranes occurs. As a rule, the pathology is a consequence of frequently recurring tonsillitis, chronic tonsillitis, scarlet fever and streptococcal diseases. In this case, damage to the epicardium is observed, which ultimately ends in scarring and thickening, which is necessary to restore and maintain the functionality of the heart.
- Myocarditis. If a person has previously suffered any infectious diseases that resulted in complications in the form of inflammation of the heart tissue, this can cause scarring. Intoxication as a result of poisoning and parasitic infestations also leads to this.
- Cardiac ischemia. This pathology accounts for 90% of all deaths from heart disease. It is the cause of numerous scars, and can also be a consequence of their appearance. This creates a vicious circle that quickly leads the patient to a heart attack or stroke.
- Myocardial infarction. In most cases, a heart attack ends in death, but if the patient received timely medical care and survived as a result of resuscitation measures, scarring will occur. This condition is the main cause of the proliferation of connective tissue, which fills the wound formed after cell necrosis.
The cause of scars can be not only the presence of one or more diseases of the cardiovascular system, but also an incorrect lifestyle, endocrine disorders, and severe stress.
The development of cardiosclerosis can be indirectly affected by the following pathological conditions:
- diabetes;
- anemia;
- obesity;
- amyloidosis;
- metabolic disease;
- premature wear of the heart as a result of heavy physical exertion;
- hemosiderosis.
In rare cases, cardiosclerosis can be detected in a child with congenital heart defects. Some adults experience a mild heart attack on their legs, thinking they are having an attack of tachycardia or angina. Sometimes a person suffering from a suffocating cough turns to a therapist for help, and the therapist, having not found the reasons for its occurrence, sends the patient for a comprehensive examination. As a result of EGC or ultrasound, cardiosclerosis is detected. In this case, the patient needs to make an appointment with a cardiologist, find out the main reason for the appearance of scars on the heart and begin treatment.
"If the scar is still with me, then I'm still alive." Jeff Green talks about the consequences of heart surgery
As a professional athlete, I always rely on my body to be in control of my brain. How does a Formula 1 driver rely on the response of his car during racing? I have always been proud of my physical capabilities. I knew that I had an advantage given by God.
But five years ago this advantage was taken away.
I had my usual NBA physical in Boston and was diagnosed with an aortic aneurysm, the main blood vessel in the body. Most people with this diagnosis find out about it only after an aortic rupture, when a human life, as a rule, cannot be saved. The Celtics doctors found me a surgeon who worked better than others with this diagnosis - Lars Svensson. In January 2012, he underwent open heart surgery.
As soon as I walked away, Dr. Svensson said, “Look at yourself in the mirror as soon as possible. You will see a completely different person. Now you will have to get used to it.” The first few days I didn't get up or look at myself. I didn’t want to take off my clothes and look at my chest. He was just lying in the room. But on the fourth or fifth day after the operation, he still went up to the bathroom, undressed and stood in front of the mirror.
I wasn't wearing any outerwear, but we often take them off during training. I was used to seeing my body naked, but this time I simply could not recognize it.
Instead of smooth and pumped breasts, I saw a long pink line from the base of my neck to the top of my stomach. The scar is 20 centimeters long. But that’s not all. Directly above the abdomen are three holes for operating tubes. The trace of them still remains on my body. Looks like a gunshot wound. Along the entire length of the scar, you could see the wire that held my chest together during the operation. At the bottom of the scar was a patch of skin that looked like a water diving board. Area with seams.
My whole body suddenly appeared completely different. All the confidence with which I built my body disappeared.
Tears flowed from my eyes. The reflection in the mirror depressed me. The realization that it would not change was even more depressing.
After a week of recovery from surgery, the Celtics sent me to Waltham for conditioning. The local recovery center was very busy; They were all getting back into shape after heart surgery, but they were all over 60. I remember one couple always occupied the treadmills next to me. They could study for about 10-20 minutes. In the first weeks after the operation, I couldn’t stay on the track for more than 5 minutes. The doctor promised that every day my performance would gradually improve, but the pressure was such that it was easy to get angry and quit everything. What can we say, if 60-year-old people could exercise on treadmills longer than I could.
I saw this couple, a man and a woman, on the simulator every day. And there was something special about their attitude towards the restoration process. Something that completely changed me.
They just never left the smile on their faces. They were constantly smiling. 24 to 7. We walked along the path and smiled. This inspired me. “You can do it, Jeff. Don’t stop,” I told myself.
I began to approach rehabilitation completely differently, but I could not forget about my fresh scar as a reminder of everything that had happened, a reminder of the situation I found myself in. I tried to smear it with a special cream, coconut oil - everything that promised to speed up the treatment. Just ask my father. He was obsessed with finding ways to eliminate the scar. I didn't want to see him. But after weeks of working on it, there was no noticeable progress. I realized that the scar was not going to go away. There was no choice: we had to somehow try to get used to it. And the best way to do this, in my opinion, was to incorporate it into your daily life. I thought that I wouldn’t be embarrassed by him. I will demonstrate. During training, they are the same when you have to take off your outerwear. That's the only way I could force myself to get used to it.
After a month of restoration work, I returned to the Celtics location. Still not back to full training, but working very hard with strength and conditioning coach Brian Du. And every time I took off my T-shirt. Some of my teammates were openly surprised at my desire to work without outerwear. One day Kevin Garnett caught me and said, “Boy, put on a T-shirt!” Paul Pierce, Courtney Lee, and even Brian Du himself told me the same thing. But I didn't care about their opinion. I continued to study bare-chested. At first, those around me were surprised by my behavior, and the scar was still fresh. But in the end they understood my motivation; realized that I needed to remember what I was aiming for with these workouts. After some time, everyone began to treat me calmly. It got to the point where some people started to think I was overly confident. Yes, baby, I'm not ashamed of my scar.
I used to hate him.
Now there was nowhere without him.
I needed to see him to remember what I went through. And the reaction of others was just an additional reminder. I started smiling. Because if the scar is still with me, then I'm still alive.
Last summer I signed a contract with a new team, the Orlando Magic. Before the first game of the regular season, my teammates started asking me about the operation and the recovery process. Elfrid Payton heard our conversation and joined in:
“Jeff,” he said. “Have you had heart surgery?!”
I was like, “Yeah, man, it’s been five years now!”
He was surprised. Immediately a bunch of questions rained down from him. And I realized that I was truly enjoying my story.
More than five years have passed since January 2012, from the moment I woke up from the operation. Since then, there has not been a day in my life without the feeling of a scar on my chest. It has healed decently, but still retained its size. It feels like something connecting my chest. The structure of the scar and its appearance will never change much. He will always be a part of my body.
Now I don't take off my outerwear so often. But my whole life changed with the acceptance of this post-operative mark. To realize that the scar that I was very afraid of at first became a symbol for the rest of my life is simply incredible.
Now in the mirror I see not just a trace from the operation. I see Iron Man.
Jeff Green
Blog navigation
Some more from ex-Orlando basketball players:
Photo: twitter.com/unclejeffgreen; instagram.com/unclejg8; Gettyimages.ru/Maddie Meyer
What is the danger?
If a person develops a scar on their heart after a heart attack, it can lead to coronary artery disease, heart failure, and an aneurysm. Much depends on what type of disease the patient suffers from. Cardiosclerosis is divided into:
- Diffuse. With this type of disease, a uniform thickening of the walls of the heart muscle occurs due to the appearance of pinpoint foci of connective tissue on them. In this case, large scars may not occur.
- Large-focal. The most dangerous type of cardiosclerosis, since it involves the replacement of large affected areas with fibrous tissue that is unable to contract. As a result of dysfunction of the cardiovascular system, serious diseases begin to develop, most often ending in death.
- Finely focal. This type of disease has a generally positive prognosis with proper treatment and systematic testing. This form is the result of a microinfarction, after which one small scar remains on the heart, which does not significantly limit the functionality of the organ.
Sometimes the appearance of a scar on the heart goes away almost unnoticed and the person continues to live without taking any measures. But it is possible to detect cardiosclerosis without undergoing special diagnostic procedures, based on the characteristic symptoms of the disease:
- cardiopalmus;
- dyspnea;
- fast fatiguability;
- constantly cold hands or feet, as well as their numbness;
- swelling of the face;
- exercise intolerance;
- blueness of fingertips.
A person who has scars on the heart suffers from severe chest pain, which can be paroxysmal (paroxysmal) in nature, looks pale due to insufficient blood supply to the tissues as a result of cardiac dysfunction.
The main consequences of cardiosclerosis are atrial fibrillation, extrasystole, heart block, stroke and heart attack. These are serious diseases that most often cause disability and death.
Surgical care for scars
Surgery is indicated only in emergency situations, when the patient is in critical condition and drug therapy is powerless. The following types of operations are carried out:
- Shunting. It consists in expanding the lumen of the coronary vessels.
- Heart transplant. Performed on patients under 65 years of age.
- Removal of the aneurysm. Under general anesthesia, a protruded area of one of the walls of the left or right ventricle is excised.
The scar after surgery heals quite quickly and rarely causes severe discomfort to the patient. After the rehabilitation period, the patient can return to a normal lifestyle, but with mandatory adherence to a special diet and further drug therapy.
A scar on the heart in medical terminology is called cardiosclerosis. The essence of the pathological process is the death of cardiac muscle cells and their replacement with connective tissue, this can happen after a heart attack or as a result of an inflammatory process. An ECG helps identify changes in the heart muscle and specify the extent of damage.
This process is dangerous for the patient’s life, since fibrous tissue is tougher in structure than muscle fibers; it is not able to contract in a rhythm synchronous with all other parts of the heart. For patients experiencing heart scarring, it is important to know the causes of this phenomenon and to prevent further changes in the heart muscle. Without appropriate help, the consequences of fibrosis can be very diverse, from heart failure and aneurysm of the lower wall of the heart to sudden death as a result of a second heart attack.
Matters of the heart, or surgery without cutting (18 photos)
Excursion to the Federal Center for Diagnosis and Treatment of Cardiovascular Diseases, which is part of the State Research Center for Preventive Medicine, located in the Kitay-Gorod area, where we will look at the operation of stenting and angiography
Angiography is a method of examining blood vessels using x-rays and contrast fluid. It is used to identify damage and defects. Without it, the operation I am about to talk about—stenting—would not have been possible.
Types of cholesterol plaques Before the advent of the stenting method, which will be discussed, doctors had only the surgical method of bypass surgery, which became popularly famous thanks to Boris Nikolaevich Yeltsin’s heart surgery in 1996 in a round operating room. I remember this incident vividly (a childhood memory), although a similar operation was performed on many famous people. Bypass surgery is a cavity operation. The person is given anesthesia, the chest is sawed open (they actually saw it, it can’t be done with just a scalpel), the heart is stopped and the artificial circulation system is started. The beating heart beats very hard and interferes with the operation, so it has to be stopped. To get to all the arteries and bypass, you need to take out the heart and turn it over. A shunt is a donor artery taken from the patient himself, for example, from the arm. Quite a stress for the body. Plaques are deposits on the inner walls of blood vessels that accumulate over years. Their consistency is similar to thick wax. The plaque consists not only of cholesterol, calcium in the blood sticks to it, making the deposits even denser. And this whole structure slowly but surely clogs the blood vessels, preventing our fiery motor, or rather pump, from delivering nutrients and oxygen to various organs, including the heart itself
Before the advent of the stenting method, which will be discussed, doctors had only the surgical method of bypass surgery, which became popularly famous thanks to Boris Nikolaevich Yeltsin’s heart surgery in 1996 in a round operating room. I remember this incident vividly (a childhood memory), although a similar operation was performed on many famous people. Bypass surgery is a cavity operation. The person is given anesthesia, the chest is sawed open (they actually saw it, it can’t be done with just a scalpel), the heart is stopped and the artificial circulation system is started. The beating heart beats very hard and interferes with the operation, so it has to be stopped. To get to all the arteries and bypass, you need to take out the heart and turn it over. A shunt is a donor artery taken from the patient himself, for example, from the arm. Quite a stress for the body. During stenting, the patient remains conscious (everything happens under local anesthesia) and can hold his breath or take deep breaths at the request of the doctor. Blood loss is minimal, and the incisions are tiny, because the arteries are entered through a catheter, which is usually installed in the femoral artery. And a stent is placed - a mechanical dilator of blood vessels. All in all, an elegant operation.
The operation was performed on Sergei Iosifovich in three stages. I found myself on the final operation in the series. It is not possible to place all stents at once. The surgical table and the angiograph (a semicircular device hanging over the patient) form a single mechanism that works together. The table moves back and forth and the machine rotates around the table to take X-ray images of the heart from different angles. The patient is placed on the table, fixed and connected to a cardiac monitor.
To make the device of the angiograph clear, I will show it separately. This is a small angiograph, not as big as the one in the operating room. If necessary, it can even be brought to the ward. It works quite simply. There is an emitter installed at the bottom, and a converter at the top (a smile is glued to it), from which the signal with the image is already transmitted to the monitor. There is virtually no scattering of X-rays in space, but everyone present in the operating room is protected. About eight such operations are performed per day.
A special catheter is inserted through a vessel on the arm or thigh, as in our case.
A thin metal wire called a conductor is inserted through a catheter into the artery to deliver the stent to the site of the blockage. I was amazed at its length!
A stent - a mesh cylinder - is attached to the end of this wire in a compressed state. It is mounted on a balloon that will be inflated at the right time to deploy the stent. Initially, this structure is no thicker than the conductor itself.
This is what the deployed stent looks like
And this is a scale model of a different type of stent. In cases where the walls of the vessels are damaged, one with a membrane is installed. They not only maintain the vessel in an open state, but also act as vessel walls.
Where do scars come from?
Heart scars form where muscle fibers have ruptured or large numbers of cells have died. The body compensates for the damage as quickly as possible - the protein fibrin is produced, which fills the damaged area. What causes lead to heart injuries:
- Thrombosis and vascular embolism. About 45% of the population over 40 years of age already have pathological changes in the blood vessels of the heart. Even the initial stage of atherosclerosis, combined with increased blood clotting, can cause thrombosis, in which a clot of coagulated blood seals the vessel bed. Some cells that do not receive the necessary oxygen and nutrients die, and local tissue necrosis occurs. Such damage poses a threat to the body, so healing occurs very quickly and with fibrotic changes in the tissue. The extent of damage to the contractility of the organ depends on the area of scar growth. An ECG helps diagnose early irregularities in heart rhythm, in particular arrhythmia. For a more detailed study of the coronary vessels, in addition to the ECG, Doppler ultrasound is prescribed. Doppler sonography shows not only the condition of the coronary vessels, but also stenosis of the aorta or inferior vena cava.
- Myocarditis. This is a group of diseases in which inflammation of the myocardial muscle tissue occurs due to infection, allergy, or other reason. Myocarditis often provokes dilatation, in which the volume of the heart chambers increases, but the thickness of the lower or lateral wall remains the same. As a result of dilatation, the heart quickly wears out and receives microtrauma in the area of the wall aneurysm. Tears and focal necrosis of the wall are replaced by fibrous fibers. The results of an ECG can reveal disturbances in the rhythm or strength of heart contractions.
- Ischemia. This is a disease in which the coronary vessels cannot meet the heart's need for oxygen, resulting in chronic oxygen deprivation. Ischemic disease often occurs with damage to the ventricles, with atrophic changes in the posterior or lower wall of the heart, and with myocardial fibrosis (especially in the area of the coronary artery). A natural consequence of ischemic disease is a heart attack. An ECG during ischemia often reveals pathological changes in the walls of the left ventricle; for a more detailed picture, ultrasound dopplerography is used.
- Heart attack. According to cardiologists, this reason is the most popular and most often provokes cardiosclerosis. A heart attack is not always accompanied by a typical clinical picture; in some people it is asymptomatic, and only an ECG can show what happened. Fibrosis in the myocardium, ventricular walls, or interventricular septum increases the risk of recurrent infarction by 45%.
A separate item can be highlighted myocardial dystrophy, that is, a condition in which the muscles of the myocardium and pericardium have atrophic changes; they are thinner and weaker than they should be according to the anatomical norm. Leads to myocardial dystrophy:
- amitaminosis;
- lack of potassium, calcium or magnesium;
- obesity;
- excessive physical activity, irrational sports;
- diseases of the endocrine system, as well as kidneys and liver.
Patients who have at least one blood relative affected by diseases of the cardiovascular system must undergo an ECG and examination by a cardiologist once a year. An ECG can prevent dangerous fibrosis of the left ventricle, protect against heart attack and premature death.
Advice! The cardiologist should be informed about existing endocrine diseases and family history. This information is important for proper prevention or treatment.
Is there a chance to prevent scarring?
The earlier scarring prevention begins, the more optimistic the prognosis. For people who have undergone surgery or been injured, experts advise:
1. Use special means to prevent wound suppuration;
2. Protect the skin formed at the wound site from exposure to ultraviolet radiation;
3. Eliminate thermal procedures and other factors that provoke the formation of keloid;
4. Use silicone preparations that normalize the water balance in the skin and promote effective tissue regeneration.
It is better to start using scar preventatives immediately after the wound has healed. In addition, you need to remember that even if the scar has already formed, its aesthetic correction is still possible.
However, here it is necessary to approach the choice of medications with extreme caution - doctors note that recently cases of self-medication of cicatricial skin changes with drugs that are insufficiently effective (simply useless) have become more frequent. As a result, scars remain, and their owners fall into despair.
Thus, scientific studies have shown that widely used preparations based on onion extract, positioned as means to prevent scars, as well as vitamin E and numerous herbal creams, not only do not help prevent the formation of scars, but can also worsen the situation. According to experts in the field of plastic surgery and cosmetology, patients who use such near-medical products only waste precious time. There is no scientific confirmation of the effectiveness of the above remedies, but there are many arguments against their use.
Thus, according to experts, preparations based on onion extract often provoke an inflammatory reaction on the skin, which only aggravates scarring. And such a popular remedy as vitamin E can cause a serious allergic reaction and the appearance of a rash, which will also lead to a worsening of the scar. Creams are also dangerous, because their use can disrupt the water balance of the skin and complicate its regeneration process, that is, on the contrary, contribute to the formation of a scar.
How to remove a scar?
The symptoms of heart scars directly depend on the disease that caused them. Within 5-10 years, fibrous replacement can occur without specific symptoms, as long as the heart manages to compensate for the volume of connective tissue and maintain contractility. Then the complaints appear:
- for chest pain;
- for shortness of breath;
- for complete or partial intolerance to physical activity;
- swelling of the face and limbs;
- for rapid fatigue.
The tips of the fingers and toes acquire a characteristic bluish tint, which signals heart failure. Treatment at this stage is aimed at protecting the heart from further damage; surgery or special medications (except cardioprotectors) are not required.
If a heart attack occurs as a result of ischemia or atherosclerosis, extensive fibrosis develops after necrosis, affecting the posterior wall, coronary vessels, often even the aortic valves. In this case, urgent drug treatment is started, which includes:
- beta blockers;
- acetylsalicylic acid;
- diuretics;
- metabolites (ATP and others);
- nitrates.
It is strictly prohibited to select medications on your own after a heart attack; you should contact your cardiologist for detailed prescriptions. Treatment should be continued until the relative normalization of well-being, not forgetting that cardiosclerosis increases the likelihood of a recurrent heart attack by 50-75%.
Fact! The scar after a heart attack continues to increase in area for 2-4 months, all this time it is necessary to maintain dynamic monitoring of the patient. Surgery may be required if the condition suddenly worsens.
Other recommendations from cardiologists regarding the treatment of fibrotic changes:
- do not overload the heart, avoid active sports and physical activity;
- remain calm, avoid emotional stress;
- support the heart muscle with a special diet.
After a heart attack, it is useful to undergo treatment in specialized cardiac centers rather than at home, this helps reduce the damage resulting from impaired blood supply to the heart muscle.
Interesting! If scars on the heart affect more than a quarter of the total volume of the organ, this is an indication for surgery.
Postoperative period
Very often, patients have gum pain after the removal of a wisdom tooth; you can read more about how dystopic teeth are removed here.
After surgery, the patient may be concerned about the following:
- Pain in the retromolar area;;
- Unpleasant and painful sensations when opening the mouth;
- Discomfort in the oral cavity;
- Swelling and hyperemia of soft tissues;
- Bleeding;
- Swelling and asymmetry of the face;
- Inability to eat food normally;
- Deterioration of general condition: weakness, fever, headache.
Surgical care for scars
In extremely severe cases, an operation is used in which a pacemaker or a cardioverter-defibrillator is installed to maintain the normal rhythm and conduction of the heart. Several more types of surgical intervention that are used for cardiosclerosis:
- Living heart transplantation from a donor. The operation is performed on people under 65 years of age without a history of serious diseases of the internal organs (which is rare, given coronary artery disease or atherosclerosis).
- Bypass surgery is an expansion of the lumen of narrowed coronary vessels. The operation is performed for severe atherosclerosis.
- Removal of the aneurysm. The bulge most often forms in the posterior wall or in the area of the left ventricle. The operation takes place under general anesthesia and consists of truncation of the protruding area.
Surgery is used as both conventional and palliative treatment. The scar after the intervention usually does not pose a threat compared to existing fibrosis.
We will be very grateful if you rate it and share it on social networks
Here are some recommendations after tooth extraction:
- Do not warm your cheek.
- Do not rinse with anything, contrary to popular belief. DO NOT RINSE. Thus, the formed blood clot is washed away and the wound opens, into which infection from the oral cavity enters.
- Do not lie down for the next hour so that the blood does not rush to your head.
- Do not lift anything heavy so that the blood does not rush to your head.
- Don't get too cold.
- No smoking.
- Don't drink alcohol.
But the most important thing in extracting a tooth is not to let it go to waste. Take care of your teeth, because a tooth is an organ like many others in our body, but it is the only one that cannot be regenerated, that is, restored. And an organ, if it is sick, needs to be treated. Although there are a lot of teeth, they eventually run out.