Determining the age of skin scars
Prescription of scars (K.I. Khizhnyakova, 1945)[1]
| Duration of the scar | Capillaroscopic picture |
| up to 2 weeks | The background of the scar tissue is clear, pale pink. The vessels are in the development stage, extend from the edges of the scar, but do not reach the center and do not anastomose. The center of the scar is pale. There is no pigmentation of the scar or surrounding tissue. |
| 2 weeks–1 month | The background is pink. The pale central part of the scar narrows. The vessels at the edges come closer to each other. No pigmentation |
| 1-2 months | The background is uniformly reddish-bluish, cloudy, the vessels are dilated, go through the entire scar, anastomose, their number increases. |
| 2-6 months | The bluishness of the background gradually decreases, the background becomes clearer, acquires a pinkish color, and scar pigmentation appears. The number of vessels gradually decreases |
| 6-12 months | The background is pale pink, clear, later brown, sometimes heterogeneous. The number of vessels decreases, they become narrow. Small folds appear on the surface of the scar. Individual large vessels are visible. |
| more than 1 year | The background is grayish-white or pale brown, sometimes heterogeneous. There are few vessels, they are located in nests. The capillaries of the skin surrounding the scar are inclined towards the scar and are narrow. |
Duration of scars (I.M. Serebrennikov, 1962)[2]
| Duration of the scar | Properties of scar | ||
| color and shades | density | other signs | |
| up to 1 month | Pinkish, later reddish with a bluish tint | Soft | Flat, tender, crusty |
| 1-2 months | Reddish, with various shades of purple, usually dark purple | Dense | Convex, sedentary |
| 2-3 months | Reddish. The blueness gradually decreases. | Dense throughout | Convex, hypertrophic in nature |
| 3-6 months | The blueness disappears. Pink color begins to predominate | Gradually softens | Convex, sometimes retracted or level |
| 0.5-1.5 years | Pale pink. A brown color of various shades appears. Later whitish, with isolated areas of brown | Slightly dense or soft. Scar density varies | The surface is uneven or smooth, at or below the surrounding tissue |
| Over 1.5 years | More often whitish (white), less often – brown | Soft, dense cords or dense throughout | Thin, atrophic, shiny, sometimes convex |
“... The color and density of scar tissue have long been used as criteria for judging the time of occurrence of skin scars. Thus, E. Pelikan (1875) pointed out that for an approximate judgment about the time of castration, it is important to take into account the appearance, color and density of scars. Brief information on the issue of determining the prescription of the GGB is available from Kornfeld (1885), N.A. Obolonsko) (1894), Wieber (1908), Ottolenghi (1910), Smith ...., 1943), Kerr (Kegg, 1946), etc. These authors note that the age of scars can only be determined very tentatively, within a few months from the moment the scars appeared.
We find the most complete information on the issue of determining the age of scars in K. I. Khizhnyakova (1945) [1]. She suggests using a number of signs when solving this issue: color, density, the nature of the surface of the scars, their edges and the degree of mobility of the scars. When using the color of scars as a criterion for their age, it is necessary to take into account several conditions: the localization of scars, their massiveness, the possibility of accidental contamination, etc. Based on his own observations of scars, mainly of gunshot origin, K.I. Khizhnyakova provides indicative information for determining the age of scars by color.
As the author notes, these data cannot be fully applied to facial scars, since due to the abundant blood supply to this area, the red color of the scars lasts much longer. K.I. Khizhnyakova notes that the density of the scar mainly depends on its age, however, here too it is necessary to take into account the localization, extent, massiveness of the scars, the method and period of healing of the damage. The approximate timing of changes in scar density depending on their age is given. Over time, the scars (after 6-8 months) become soft and subsequently their consistency does not change. K.I. Khizhnyakova comes to the conclusion that the age of scars after gunshot injuries can be determined approximately within 1.5 years.
CM. Sidorov (1954)[3] examined 84 patients with gunshot wounds to resolve the issue of how long ago the wounds were. He believes that scars up to 2 months old are soft, from 2-3 months to 4-6 months they are slightly dense, and after 6-12 months they are dense. K.I. Khizhnyakova, who studied a significant number of scars after gunshot wounds (bullet and shrapnel), came to the conclusion that the greatest density of scars is observed up to 3 months, and then it gradually decreases (from 3 to 6 months) and after 6-8 months the scars become soft.
It should be noted that in small scars, the formation of which ends much sooner, the color change occurs faster than indicated by I.M. Serebrennikov. Scars that appear at the site of skin damage from the cutting of surgical sutures quickly become white and hardly noticeable, while in the main scar the process of its formation and corresponding color changes take place for a long time. The color change is due to the general formation of scar tissue. The faster the formation occurs, the faster the color changes. In very extensive scars, color changes may occur more slowly than indicated by I.M. Serebrennikov.
A known influence on the color of the scar is its localization. Scars located in the face and lower extremities, due to the peculiarities of blood circulation, retain a bluish tint for a very long time. Changes in scar density occur, judging by our data, as follows. Fresh tripe usually has a soft consistency. Around the end of the 1st month, the volume of scar tissue increases, the scar begins to protrude above the skin level and evenly thickens, becoming dense. Scars can remain in this state for various periods of time - until the end of the 2nd or even 3rd month. Older scars gradually soften and flatten. In such scars, all these cyclic changes that are normal for a scar are poorly expressed and it is often not possible to notice changes in density by touch.
It should be emphasized that the density and nature of scars depend not only on their age, but also on the amount of fibrous tissue formed during the formation of the scar, the depth of the former damage and localization. In massive scars of considerable length, the density of scar tissue throughout the scar is often heterogeneous. Often scars, having become dense, remain in this state for many years. In some cases, this is due to hyalinosis of scar tissue. The conclusion about the age of scars is based on such objective data as the color, density and nature of the scar tissue. Capillaroscopic examination of them can also help determine the age of the scar. In addition, you need to take into account various medical and investigative documents, which often indicate the time of receipt of certain injuries. The expert must also critically take into account such subjective data as the testimony of the examinees about the time of scar formation. Often he has the opportunity, without establishing the exact age of the scars, to indicate in the conclusion that they appeared at different times. And such a conclusion can be very useful for investigative authorities. It is impossible to recognize as scientifically substantiated the still encountered conclusions of forensic experts, which accurately indicate the age of scars after the end of their formation (for example, “the age of the scar is 5 years, 10 years,” etc.). Based on the study of only the external properties of the scar, such conclusions should be considered erroneous and scientifically unfounded.” [2]
Wound healing process and scar care
After surgical interventions, scars always remain. Despite the surgeon's desire to minimize the size of the scars with precision surgical techniques and the use of suitable suture material, the scar may remain noticeable and therefore negatively perceived by the patient. Individual differences in the healing process and scar maturation play a major role in the final appearance of a scar. But although the features of this process are given to us genetically, there are opportunities to positively influence it.
Wound healing and scar maturation.
The process of scar maturation lasts about a year. The fastest and most noticeable changes are observed in the first three months, then the scar changes very slowly. Immediately after surgery, the scar is thin and soft, but after 2-3 weeks in most cases it turns red, thickens, becomes more visible and hard. Then it gradually matures, the scar turns pale and becomes softer. The reason for this development of the scar and wound condition is the essence of the healing process. With an open wound, the body mobilizes and tries to close the wound as quickly as possible. Therefore, the wound will close with excess connective tissue and blood vessels. The scar at this moment is harder and redder. After the wound heals, a long-term process of gradual resorption of excess connective tissue and closing of excess vessels begins, the scar fades and becomes softer. Since the wound has already healed, this process is not urgent for the body and lasts for many months. The final appearance of the scar can be assessed one year and sometimes two years after surgery.
Both the patient and the surgeon want the scar to be as inconspicuous as possible, so today we'll talk about the types of scars and how comprehensive scar care can help speed up the maturation process.
Physiological scar
This is a normal scar that remains after healing, which occurs as described above. The thin, soft scar will initially become hard and red, but will become soft and pale over time.
Keloid scar
This is a hypertrophied, raised, itchy scar that expands beyond the boundaries of the original wound. It can be red, even purple, and there are sensations of itching and burning. Most often, such a scar appears above the sternum, on the shoulders, earlobes and is more common in patients with darker skin types. It often occurs even long after the wound has healed. The reason has not yet been explained.
Hypertrophic scar
Often such scars are confused with keloids, but hypertrophic scars do not extend beyond the boundaries of the original wound. In appearance and properties they are similar to keloid scars, but they are less protruding above the surface of the surrounding skin. Frequent areas of appearance are the same as for keloid scars. The reason for their occurrence has also not yet been explained.
Atrophic scar
Actually, this is the antipode of a hypertrophic scar. The scar, which lies below the surrounding skin, is often wide and soft. Atrophic scars are relatively rare.
Basic care methods
It is useful to lubricate any scar with fat. You can use unsalted lard, Calcium pantothenicum ointments, Infadolan, Nivea, Indulona, Calendulova and a number of other drugs. The main thing is that the cream is thick enough, with a minimum of water. The scar must be protected from sunlight for at least 3 months after surgery, but it is better to withstand it for six to a year without sunbathing. Creams with a protective factor of 20 or more are suitable. Intense solar radiation irritates the scar and can cause its growth - hypertrophy. The scar may also have more melanocytes (colored cells) and the scar may appear dark—hyperpigmented.
Pressure massage
Applying constant pressure to the scar has been proven to prevent the development of a hypertrophic scar. Pressure massage is suitable for all types of scars, on the one hand, as a prevention of the occurrence of a pathological scar, on the other hand, to accelerate the maturation of the scar. Proper pressure massage technique is very important. We press quite intensely on the scar (1-2 weeks after removing the sutures) with our finger so that the nail bed of the pressing finger deviates, which will manifest itself as whitening. We press on one place for 30 - 60 seconds, then release the pressure and move the finger to another part of the scar. We continue in this way until we massage the entire scar. There is no need to rub the scar with your finger, just apply pressure. We perform massage at least 5 times a day. Its effect is noticeable after 2 - 3 months.
Ointments and creams
Many different creams and ointments with a positive effect on scars appear in advertisements (for example, Contactubex, Cicatridine, etc.). However, the effect of their use has not been proven, and sometimes you can encounter an allergic reaction to them. However, some people may benefit from these ointments. It should still be noted that the use of any fatty cream has a beneficial effect on the scar.
Sealing scars
The seams can be sealed with a strip of hypoallergenic plaster. Its effect is to provide long-term light pressure and at the same time protect the scar from being stretched by surrounding tissues during movement. That is, to some extent it prevents stretching of the scar. In areas where seams are subject to a lot of stress, such as near joints, taping is a more suitable maintenance method than others. The condition, of course, remains good skin tolerance to long-term wearing of the patch.
Silicone gels
The beneficial effect of silicone gel on scars has been sufficiently confirmed by research. On a healed scar, you can apply special silicone plates (Silipos, Topigel, Mepiform) or apply silicone gel in the form of an ointment (Dermatix Sigel, Strataderm, Xeraderm, etc.). Silicone plates are self-adhesive or secured with a hypoallergenic patch. Some silicone sheets also contain minerals that lubricate the rumen. Silicone gels accelerate the maturation of scars and prevent their hypertrophy. The gel can be applied to the scar for 20 hours every day. In very rare cases, intolerance to the gel may occur; an allergy to it has been observed in isolated cases.
Laser
A certain type of laser can have a very good effect on the maturation of scars. In most cases, it is available at cosmetic laser centers. However, if the scar matures normally, then there is no need to use a laser.
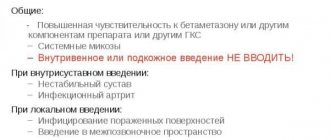
Corticoids and other drugs
These are hormonal medications used in cases where scars do not respond to the above methods of care and treatment. Medicines can only be recommended after examination by an experienced specialist. Injections of a corticoid substance are repeated into the scar, about once every 5 to 6 weeks. The effect can be enhanced by simultaneous application of corticoid ointment to the scar.
If the pathological scar does not respond to any of the above treatment methods, you can try more invasive methods: laser, cryotherapy (freezing) or surgical excision of the scar. After these invasive interventions, it is necessary to take intensive and long-term care of the scar to prevent the pathology from renewing.
Scar formation and its types
Scar formation is a serious problem for the client of a beauty salon and for the specialist himself. In addition, people often come to us who have already acquired a scar and want to get rid of it, and cosmetologists also try to help them with this. In order to prevent the formation of scars and promote their healing, or at least give them a more aesthetic appearance, you need to know what scars are and how they form.
A scar is a consequence of the skin healing process, during which damaged tissue is replaced by connective tissue. In everyday life, scars are called scars; there is no difference in the meaning of these concepts. There can be many reasons for the occurrence of scars, these are any influences that damage the skin: mechanical damage, burns, skin diseases (such as post-acne), the consequences of surgery or complications after unsuccessful cosmetic interventions.
The process of scar formation
The scarring process is normal for the body and it goes through the following stages:
- Inflammatory process and epithelization. This stage lasts from the moment of injury for the first 7-10 days. During this time, skin swelling and inflammation should decrease. At this time, the edges of the wound gradually come closer together, granulocyte tissue is formed, and there is no pronounced scar. At this stage, complications such as tissue infection and wound dehiscence are possible. In the case of such complications, the possibility of forming a thin, inconspicuous scar becomes more difficult. Therefore, to prevent complications, atraumatic sutures can be applied, the wound is disinfected and frequent dressings are performed. The edges of the wound should not be allowed to diverge, so physical activity that could re-damage the injured area should be limited.
- Formation of a “young” scar. This process lasts from the end of the first stage until a month after the injury. During this period, granulation tissue, which consists of collagen and elastin fibers, is actively formed. At this stage, the scar is still easily stretchable and the likelihood of re-injury is high, so physical activity is still limited. At the site of scar formation, there is an increased blood supply, so it is bright pink, loose and immature.
- Formation of a “mature” scar. This scar forms about three months after the injury. During this period, collagen and elastin fibers grow into bundles, lining up in a certain direction. At the same time, the blood supply to the injured area decreases, and the scar finally turns pale and thickens. Such a scar is less at risk of re-injury; it reliably protects the affected area. However, if repeated traumatization does occur, there is a high probability of complications, such as the formation of a keloid scar.
- Scar transformation. The formation of a scar in the form in which it will accompany us in later life occurs within a period of up to one year after the injury. At this stage, all the vessels that supplied it finally die off, the collagen fibers are stretched and the scar becomes as dense as possible and turns pale. When the final picture of how the scar has formed is already visible, the doctor can develop tactics for its correction. After the end of the one-year period of scar formation, changes in its structure may continue to occur, but they will be very slow and almost imperceptible.
Types of scars
The deeper the tissue is damaged, the more pronounced the scar and the more difficult it will be to heal. The surface layers of the epidermis have much higher rates of regeneration. If the scar heals without complications, a normotrophic scar will form. It is flat in structure and does not differ much in color from the surrounding skin. The appearance of complications at any stage of scarring threatens the formation of a pathological scar. In order to choose the right method for scar correction, you need to understand the nature of the scar.
Normotrophic scar . Appears as a result of shallow injuries, professional surgical incisions, but only if the scarring process is carried out correctly. Such scars do not cause any particular inconvenience. Their level of elasticity is close to that of normal skin, and the color may differ only slightly. Moreover, such scars do not protrude above the surface of the skin and do not form indentations, but are at the same level. Normotrophic scars do not always require any intervention to correct them. If necessary, they are eliminated using superficial chemical peels or microdermabrasion, which significantly improves the aesthetic appearance of the scar.
Atrophic scars . The peculiarity of such a scar is that it is located below the level of the surrounding skin. Such changes in the skin are typical after removal of moles, papillomas, and acne. This type of scar also includes stretch marks. They are formed due to a decrease in the level of collagen synthesis, the skin becomes more flabby. Such scars or pits are visible to the naked eye and cause inconvenience. Therefore, aesthetic medicine is developing a wide range of methods for treating this phenomenon:
- mesotherapy;
- microdermabrasion;
- chemical peeling;
- laser therapy;
- enzyme therapy;
- cryotherapy;
- surgical excision;
- use of creams, ointments and gels for scars: Contractubex, Mederma, Dermatix Ultra gel, Fermenkol, Zeraderm Ultra cream, Scarguard liquid cream, Spenko silicone plates, Kelo-cote silicone gel and spray, Kelofibrase.
Hypertrophic scars . This type of scar protrudes above the surface of the skin and is pink in color. This scar may noticeably shrink and become normal within two years, but there is no point in waiting that long when there are many ways to improve its appearance faster. Such scars are treated with injections of hormonal drugs such as Kenalog or Diprospan. In addition, chemical peels, cryotherapy, dermabrasion and laser resurfacing are used. Electrophoresis and ultraphonophoresis are also used. The best cosmetic effect is achieved by surgical intervention in which the scars are excised.
Keloid scars . This is a tumor-like growth of the rough fibrous connective tissue of the skin. Their formation is accompanied by itching and burning; they have a clear outline and protrude above the surface of the skin. Its peculiarity is that it is the least amenable to correction and the likelihood of relapse is high. However, there are still ways to successfully treat such scars.
For productive treatment, the type of scar must be accurately determined. This is where the difficulty arises in differentiating keloid scars, because they are very similar to hypertrophic ones. However, keloid scars extend beyond the immediate injury. The highest probability of scarring occurs in the area of the ears, chest, and sometimes joints. The process of formation of a keloid scar is different from others. Keloid scars are divided into young - from 3 months to 5 years and old - more than 5 years. If young keloids are smooth, shiny and red, then old ones become pale, wrinkled and their central part may sink inward.
Scars cause a lot of inconvenience, especially their aesthetic component. That is why it is worth taking measures to improve their appearance. The main component of successful treatment is understanding the nature of its occurrence and correctly determining the type of scar.
Anna BUNYAK
Premium WordPress Themes Download
Download Premium WordPress Themes Free
Download Best WordPress Themes Free Download
Download WordPress Themes Free
online free course
Scarring
Phase of epithelization and reconstruction (maturation) of the scar
Collagen accumulation within the wound reaches its maximum within 2-3 weeks after injury. During the normal course of the wound process, capillary density and the number of fibroblasts decrease (Fig. 25-5).
The wound loses its pink color and becomes more and more pale. Collagen undergoes constant remodeling. 3 weeks after injury, a balance is established between the activity of collagen synthesis and lysis processes, after which tissue reconstruction (remodeling) begins in the developing scar. During this phase, the strength of the scar tissue increases. It continues to “mature” and gradually achieves the same collagen ratio as in normal skin. Immediately after the formation of the scar, its restructuring begins - the formation of elastic fibers and the development of a new fibrous network occurs, the water content in the scar tissue decreases.
Epithelization is the process of migration of keratocytes, which occurs from the edges of the wound at a speed of 1-2 mm/day. Epithelization of the wound begins simultaneously with the formation of granulation tissue. Normally, restoration of the epithelium begins within a few hours from the moment of injury, and complete epithelization of a initially sutured wound occurs within 7-10 days. The epidermis serves as a protective barrier that prevents water loss and allows other body cells to remain in a liquid environment. It serves as a barrier to bacteria. After epithelization there is no longer any need to protect the wound from water. At the same time, it should be remembered that newly developed epithelial cells are not firmly attached to the dermis, are easily damaged when dressing and require protection.
Bacteria, proteinaceous exudate from capillaries and necrotic tissue significantly delay epithelization. Delayed epithelization leads to a deeper and longer-lasting inflammatory process and thereby contributes to the formation of a rough or hypertrophic scar.
The final phase of wound healing, depending on the morphology of the tissue, lasts from several weeks to a year. The duration of the maturation phase depends on various factors, including the genetic characteristics of the patient, his age, location of the wound, type of injury, and the duration of the inflammatory process.
Despite the relative stabilization of biochemical reactions during the first 2 weeks, wounds have only 3-5% of the initial strength of the tissue at the wound site or about 7% of the safety margin after the formation of the postoperative scar is completed. During the 3rd week, wounds acquire about 20% of their final strength, and after a month - 50%. This 50% is only 35% of the original strength of the fabric.
It should be noted that this figure never exceeds 80% of the strength of healthy, undamaged tissue, even after 60-150 days, when the final formation of collagen fibers in scar tissue is completed. Although the wound never reaches the strength of intact tissue, the scar formed during the healing process is rebuilt over time and the collagen fibrils, which are randomly located in the process of fibroplasia, begin to change location depending on the forces of external influence.
As the water and mucopolysaccharide content in a healing wound decreases, collagen fibrils undergo compression and cross-links become stronger. Within 3 months, the scar becomes flat, soft and light. Collagen fibrils are denser, become denser, blood vessels narrow and disappear. The severity of the forces acting on the wound is very important in wound healing. This determines the amount of scar tissue that forms. In this way, the wound is transformed from tissue rich in capillaries and cells into a relatively avascular scar, poor in cellular elements, consisting of durable collagen tissue.
The final stage of wound healing is epithelization of the wound surface. Epithelial regeneration becomes an essential aspect of tissue restoration, providing an effective barrier against bacterial invasion, necessary function and appearance. This process involves mobilization of basal cells from their attachment to the dermis, migration to the site of injury, mitotic proliferation, and replacement of precursor cells. Cellular function is restored through differentiation.
The movement of epithelial cells through the damaged area continues as long as there is a shortage of them in the wound. The fundamental process that initiates cell division and migration is not fully understood. However, it is known that it continues until the epithelial cells come into contact with similar cells on the other side of the wound (the phenomenon of “contact” inhibition).
The end result of an uncomplicated wound healing process is the formation of a tender scar with little fibrosis, minimal in the presence of wound contraction, and a return to almost normal tissue structure and organ function.
The course of the wound process described above is typical for wounds resulting from a simultaneous external influence of a damaging factor. With prolonged adverse effects, the wound process becomes chronic. Typically, this is how tissue damage occurs in diabetic foot, bedsores, ischemic and venous trophic ulcers of the leg. The pathophysiology of chronic wounds is complex and varied, but they have one common feature - long-term inflammation, which leads to extensive tissue damage and impedes healing.
Healing of different wounds occurs as a result of the same processes. Of course, the division into phases is to a certain extent arbitrary, but it reflects the chronological sequence of events characterizing the process of wound healing.