Dear friends, a lot has been written about the removal of figure eights, wisdom teeth, impacted and not so much (for example, here>>, here>> and here>>). In principle, the manual for this surgical intervention is well known and understandable to you.
Today I invite you to talk about something less known and even more obscure, namely, what happens in the surgical area after we have sutured the patient and sent him home. Understanding these processes is important both for doctors (if we are truly looking for ways to reduce trauma and improve the safety of surgical operations) and for patients (in order to understand why medications are prescribed and recommendations for postoperative regimen are given).
Well, in the end, it is not “golden hands” that determine a good surgeon. Because a manual, a simple sequence of movements, can be taught even to a monkey - and this will not make it a doctor. A good surgeon is, first of all, a “golden head” who knows how to think, analyze, interpret and make the right decisions. Therefore, in all my lectures, reports and seminars, I encourage doctors to train their heads. And the hands... will begin to work correctly only after the head works correctly.
How incomprehensible our topic is today, I will show you, dear friends, with a simple example.
Just now I had two lovely girls at my reception. The same. Gemini, that is.
With the same problem - impacted wisdom teeth and associated bite pathology.
In preparation for orthodontic treatment, we decided to remove all of my wisdom teeth. First on one side, then on the other.
The girls had operations one after another, with a difference of 20 minutes. Each intervention took no more than 15 minutes. As they say, without any special features.
The twins were given the same recommendations on the postoperative regimen and made the same prescriptions. A day later, I was invited for the first postoperative examination.
Let me emphasize once again: two completely identical (including genetically) girls, two identical operations, recommendations, appointments…. But look at the symptoms of the postoperative period:
Another day later:
How is it that one of them has significant swelling and pronounced postoperative symptoms, while the second is only slightly swollen? What caused this difference? And what influenced the development of symptoms in each of the two identical cases?
I will answer you honestly:
Of course, the most general processes occurring in our body, for example, breathing, muscle function, metabolism, regeneration, etc., have been well studied - for this we have physiology, pathophysiology, biochemistry and many other useful sciences.
But we are not yet able to explain why, all other things being equal, one person easily endures even severe injuries, while another almost dies from the slightest scratch. Our body is still a mystery. We now know more about space and the structure of the Universe than about how our body works. That’s why – who knows.
And yet, let me share with you what allows us to predict the symptoms of the postoperative period and, as a result, to correctly plan surgical interventions and make them safe. No, seriously - in our clinic we could even do a kidney transplant, but it’s not a fact that the patient would survive - we don’t know how to plan such treatment and predict its consequences. But we perform a lot of osteoplastic surgeries - more than three hundred in 2018, and our failure rate is extremely small, below 2%. And all because we understand osteoplasty at the level of physiology, histology, pathoanatomy and biochemistry, and this gives us the opportunity to correctly assess the risks and choose the safest and most effective method of bone tissue augmentation.
So, we just finished the surgery, no matter what, and placed the last suture ligature.
We looked around, checked the integrity of the sutures and sent the patient for a control X-ray (optional).
Firstly, that any surgical operation is an injury . Yes, the body almost doesn’t care whether your tooth was knocked out in a fight, or whether it was carefully removed by a dentist in a fight. The processes that occur after an injury and a comparable surgical operation are almost identical.
Secondly, any surgical wound in the oral cavity is infected . Simply because a healthy person, even with perfect hygiene, has a whole zoo of all sorts of microbes living in his mouth, and during the operation they inevitably end up in the operation area. It is impossible to create absolutely sterile conditions during operations in the oral cavity. Yes, and you don't need to do this.
Fortunately, over millions of years of evolution, the human body has learned to solve these two problems.
The response to any injury (including surgery) is an adaptive reaction – inflammation. It is a cascade of processes moving from one to another, beginning with the identification of foreign agents and ending with the launch of the restoration of damaged tissues.
In addition, our body has learned to coexist so peacefully with its entire intraoral zoo that we even call it “normal microflora of the oral cavity.” To do this, he created a completely unique system of local immunity, which is not so easy to break through. Well, judge for yourself - the emergence of an infectious-inflammatory focus in any of the bones of our skeleton is, at a minimum, fucked-up osteomyelitis, with all that it implies. At the same time, a hilar cyst or granuloma can exist in the jawbone for a long time - nothing more than a “bubble with microbes,” but we don’t even notice it.
And then comes the most interesting part.
After surgery, an inflammatory process develops, consisting of three successive phases: alteration , exudation and proliferation . It is often impossible to draw a clear boundary between them, however, all these phases of varying degrees of severity are characteristic of inflammation of any origin. Knowing them, you can easily explain all postoperative symptoms and possible postoperative complications.
Caring for sutures and wound surfaces
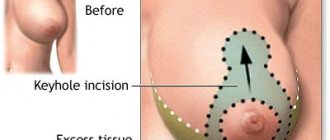
The main postoperative risk is wound infection. After intimate plastic surgery, this danger is high, due to the proximity of the urethra and anal area. To avoid infection and speed up healing, you should carefully care for the wound:
- If in the first days after the procedure a small amount of ichor is released from the wound, it is necessary to treat the tissue with a healing ointment. In this case, it is undesirable to apply the healing composition directly to the mucous membranes. It is better to treat sanitary pads with ointment.
- After each visit to the toilet, you should apply an antibacterial solution to your genitals. For this purpose, special pharmacy sprays are used. They should be used 7-8 times a day.
- To avoid overheating the wound and causing infection, it is advisable to change sanitary pads frequently. This will speed up swelling and healing.
7-10 days after the intervention, postoperative wounds heal. Complete tissue healing takes at least a month.
Proliferation
Yessss! We all live and work for proliferation. This is the most anticipated phase of inflammation for any surgeon. It is characterized by the migration of cells and the biologically active substances that control their division and differentiation, as well as the launch of regeneration processes of damaged tissues. In fact, proliferation very smoothly turns into regeneration, which, in principle, is the basis of such treatments as bone tissue augmentation, implantation and gum surgery.
During the proliferative phase, active movement of precursor cells (fibroblasts, osteoblasts) occurs. This movement is controlled by hormone-like substances (about thirty compounds in total, the most famous group for dentists are bone morphogenesis proteins, BMP-I, BMP-II), formed during the previous phases of inflammation. In parallel with migration, the processes of division and differentiation of cells already located in the area of injury and surgery are launched.
In fact, proliferation is the beginning of the regenerative process, with the help of which our body restores its integrity, and at the same time integrates implants and biomaterials. We have talked about regeneration many times, for example, here>>, here>> and here>>, and we will talk a lot more as we study osteoplastic surgery and implantation. And we will consider it as a separate process, in which inflammation is just a starting point, an initiator, nothing more.
Unfortunately, not all tissues are capable of proliferation. Thus, nerve fibers practically do not regenerate, but they have good intracellular restoration capabilities (hyperplasia and hypertrophy). The proliferation rate of different tissues and cells also differs: for example, connective tissue itself regenerates much faster than bone tissue, therefore, when growing bone tissue, in order to avoid growth into the graft, we separate it with a barrier membrane. Read more about this here>>
You need to know the following about the proliferative phase:
– proliferation will not occur without the two previous stages of inflammation, alteration and exudation. In other words, there is no creation without prior destruction.
– all components necessary for proliferation appear in the postoperative wound , thanks to the two previous phases of inflammation.
– in general, proliferation requires cells and substances that control the migration, division and differentiation of these same cells.
– proliferation can be considered as the initial stage of regeneration. It turns out that there is no regeneration without an inflammatory process preceding it.
– proliferation is a nonlinear process. Over time, the rate and intensity of proliferation slows down.
– it is impossible to control proliferation. Almost impossible. Cells cannot be forced to migrate, divide, and differentiate faster than nature intended. The maximum that we, doctors, can do is to calmly and confidently guide the patient through the two previous phases of postoperative inflammation, so that proliferation also occurs calmly and confidently.
When can you have sex?
After the operation, you need to abstain from intimacy for at least 3-4 weeks. In the first days, even arousal can have a negative effect, as this increases blood flow to the genitals. The longer the period of abstinence lasts after surgical correction of the intimate areas, the faster the healing will occur.
After rehabilitation, the patient does not lose sensitivity in her intimate areas. Most women who decide to undergo correction, on the contrary, note an increase in the quality of sexual life and increased pleasure from intimacy with a partner. This is due to physical and psychological factors.
Limitations after intimate plastic surgery
For at least a month after surgical correction, the following restrictions must be observed:
- refuse to take hot baths, visit baths and saunas;
- It is undesirable to wear tight synthetic underwear;
- Do not use hygiene products containing aggressive chemical components;
- limit stress, avoid heavy physical labor and sports;
- You should not drink alcohol or take medications that affect the blood coagulation system.
Doctors recommend spending more time in a supine position during the first month of rehabilitation. This promotes blood flow from the genital area and quickly reduces swelling. It is also advisable to maintain a sleep-wake schedule, avoid stress, and adhere to the principles of a healthy diet.
Will the scars be visible?
The purpose of intimate plastic surgery is to correct physiological and cosmetic defects of the genital organs. A qualified gynecologist surgeon will perform the procedure so that its traces will be completely invisible. To avoid scars, preference should be given to the surgical method of correction. The laser technique, popular today, causes tissue hardening, coagulation of blood vessels and the formation of thickened dark zones.
At the Center for Aesthetic Intimate Surgery in St. Petersburg, all operations are performed by experienced surgeons after a thorough study of the patient’s problem. This allows you to choose the right technique and avoid postoperative complications. Throughout the entire rehabilitation period, the clinic’s doctors support the patient and monitor her condition.
All surgical interventions are performed on an outpatient basis, which involves staying in the recovery room for two to four hours under the supervision of the operating physician and anesthesiologist. After the operation, it is necessary to follow a number of recommendations that depend on the type of surgical intervention.
Exudation
The alteration smoothly passes into the exudative phase, during which plasma and blood cells, tissue macrophages, leukocytes, etc. enter the cavities and/or intercellular space formed during the injury. Edema of the intercellular substance develops, in which active phagocytosis and a whole complex of biochemical reactions are still taking place, leading to the formation of exudate - a liquid very similar to blood plasma, but containing a large amount of protein, oligopeptides, whole and destroyed blood cells and tissues, etc. At this moment, patients often note: “Doctor, something is flowing from my wound!” This is the exudative phase of inflammation, a common, in general, stage of the postoperative period.
Another thing is that the nature of the exudate is an important sign of whether everything is in order with the postoperative wound. Most often, we observe serous or serous-fibrinous exudate - a translucent liquid of varying degrees of turbidity, slightly similar in taste and smell to blood. Such exudation is a normal phenomenon, indicating that everything is in order with the operation area, postoperative inflammation is proceeding as it should.
And sometimes nothing comes out of the wound at all - all the excess accumulates in the cellular spaces and cavities, gradually disappearing due to osmosis. This happens when we seal a postoperative wound, for example, during osteoplastic surgery.
In case of loss of control over the rehabilitation period, pus appears - exudate with a high content of protein, leukocytes, dead tissue cells and microbes. Its main difference between more or less acceptable wound discharge is its viscosity (very thick), transparency (opaque) and odor (unpleasant). The pus coming out of a postoperative wound does not pose any serious danger, because this is also a way of removing all sorts of nasty things from the body. As the nastiness becomes less, suppuration decreases and even stops completely. If pus, having formed, does not leave the wound or accumulates in the cellular spaces and cavities, this is already an abscess or phlegmon, which may require separate surgical treatment.
It is exudation that explains the increase in postoperative swelling on days 2-3 after surgery - at first, everything seems to look normal, but then the swelling increases, reaching its maximum, usually on days 2-3 - and many are very worried about this. Moreover, some patients evaluate the quality of the surgical treatment performed by the size of the resulting edema - they say, if there is no edema, then “the surgeon is great,” and if it is too large, then “the doctor did something weird.”
Meanwhile, the severity of edema is influenced by many factors, from the traumatic nature and duration of surgical intervention to the lability of the microvasculature, hormonal levels and the general condition of the body. And, unfortunately, it is not possible to reliably predict the size, period of formation and disappearance of edema. Look at the twins at the beginning of the article - it would seem that they are the same people and have the same operations - but how different the postoperative symptoms are!
In general, you need to know the following about the exudative phase of inflammation:
– there is always exudation, even when “nothing flows” from the wound. Swelling of the postoperative wound area is explained, among other things, by the accumulation of exudate in the soft tissues.
– not every exudate is pus. The flow of fluid from a wound is not at all a reason to undo the stitches and immediately pick and rinse something there. In itself, exudation is not dangerous.
– purulent exudate does not form immediately after surgery. It takes time for pus to form. Therefore, if your cheek is swollen after surgery, this does not mean that there is pus there.
– swelling of soft tissues is not necessarily a “flux” in the popular sense of the word or a phlegmon (abscess) in the medical sense. If the postoperative period is favorable, it passes within a few days. Only a doctor can catch the moment at which “something goes wrong” - that’s why it is important to be monitored after surgery.
– the severity and magnitude of postoperative edema are difficult to predict due to the many factors influencing them.
– the size and severity of edema cannot be used to judge the quality of the surgical treatment performed.
In addition to removing inflammatory agents from the body, the exudative phase has another important function; it facilitates the migration of cells and biologically active substances that trigger the next phase of inflammation - proliferation.
If hysteroscopy is performed
- Appear for the results of histological examination in 10-21 days, information about the timing and possibility of obtaining on the website, section histological examination, or by calling (812) 275-21-53.
- Sexual rest for 2 weeks.
- Barrier contraception (condom) 1 month, for patients of reproductive age.
- Restriction: pool, sauna, bath 2 weeks, shower allowed.
- Limiting physical activity for 24 hours, for 2 weeks a gentle regime, which involves the presence of normal loads.
- The presence of scanty bloody discharge from the genital tract for 2 weeks is considered normal.
- It is mandatory to take broad-spectrum antibacterial drugs; the specific drug is indicated in the discharge certificate.
- If there is bloody discharge from the genital tract more than 3 sanitary pads per day, increased pain in the lower abdomen, an increase in body temperature above 37.5 degrees, call your doctor by phone: +7-921-311-45-68.
Recovery after surgery
The length of the recovery period after bariatric surgery depends on the type of procedure. Below are the average time ranges:
- Recovery period: 3 days - 6 weeks until complete recovery
- Hospital stay: from returning home on the same day to 5 days
- To work: from 4 days to 3 weeks
- Pain syndrome: from mild discomfort to manageable with medication
- Diet: Slow transition from clear liquids to solids
- Activity: walking – no restrictions, physical activity – limited for 2 months
Be sure to consult with your surgeon in person before surgery to make your final decision and ask any questions you may have regarding diet, exercise, and lifestyle.
Familiarity with the hospital and facility where your surgery will be performed will help you better adapt to the environment during your hospitalization.
- The day before surgery, have lunch with your usual food and eat a light dinner at 6 pm.
- Next, you will need to observe hunger.
- Liquid intake should be stopped at 10 pm on the eve of surgery and not drunk until surgery.
The day of your surgery is a very important day for you, so do your best to avoid any stress and avoid rushing or stress. Set your alarm for an earlier time to give yourself enough time to prepare.
Your surgery will last from 1 to 4 hours depending on the type of procedure:
- Installation of VZHB from 30 minutes to 1 hour
- Laparoscopic adjustable gastric banding: less than 1 hour
- Laparoscopic longitudinal gastrectomy: about 1-2 hours
- Laparoscopic mini-gastrobypass surgery: 1.5-2 hours
- Laparoscopic gastric bypass: about 2-3 hours
- Laparoscopic biliopancreatic bypass – about 2.5-4 hours
According to modern standards, our specialists will use the following medications before surgery:
- Standardized anesthesia with modern drugs
- Subcutaneous injection of local anesthetic before making the incision
- Avoid the use of prophylactic nasogastric tube placement
After the procedure, our team of specialists will:
- Closely monitor your condition and take care of your comfort.
- Use standardized medications to relieve pain and nausea
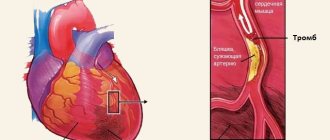
- Use standardized methods to prevent deep vein thrombosis
From 2 to 24 hours after surgery - pain relief - start of activation
On the first day after surgery, you will be closely monitored by medical staff.
- Pain syndrome: administration of painkillers on demand
- Diet: fasting, a couple sips of water 2 hours after surgery
- Movement: You may feel weak or tired, but this will begin to subside as you begin your new diet and activity regimen.
- Start by sitting up in bed
1 day after surgery - drinking clear liquids and walking around the department
Here's what you can expect the day after weight loss surgery:
- Moderate pain in the area of postoperative wounds and muscle discomfort from being on the operating table. Pain in the neck or shoulders is also common.
- Gradually the pain syndrome will pass. You will be able to receive pain relief as needed.
- Diet: During your hospital stay, you will drink clear liquids in small sips. Laparoscopic Adjustable Gastric Banding: Clear Liquids Can Be Started
- Activation: walks within the department at least 3 times a day
- Breathing exercises
- One week after surgery - start taking pureed foods
In the second week after surgery, you will switch to pureed foods.
At 3-4 weeks after surgery, you will gradually return to your normal eating habits, but your diet and the amount of food you eat will be significantly different from what you ate before weight loss surgery.
If you have undergone vaginal plastic surgery
- Turnout in 7-10 days.
- Sexual rest for 1 month.
- Restriction: pool, sauna, bath 2 weeks, shower allowed.
- Limiting physical activity for 3 months.
- Do not sit for 1 month.
- If there is bloody discharge from the genital tract more than 3 sanitary pads per day, increased pain in the lower abdomen, an increase in body temperature above 37.5 degrees, call your doctor by phone: +7-921-311-45-68.
- Treatment with furacillin solution (5 tablets per glass) or chlorhexidine solution (aqueous).
- It is mandatory to take broad-spectrum antibacterial drugs; the specific drug is indicated in the discharge certificate.
- 2 weeks after surgery, it is recommended to perform Kegel exercises (list and technique) to strengthen the vaginal muscles.
What happens?
And it turns out, friends, a very interesting thing.
We are all terribly afraid of inflammation. “Doctor, do I have inflammation?” – patients ask, pointing out swelling the day after surgery. We worry about developing swelling, increased body temperature and other normal postoperative phenomena. We believe that everything - edema, exudation, hyperthermia, and inflammation - are complications of the postoperative period. I will say more - in my practice there were cases when the doctor removed implants a day after installation, citing the “flux and inflammation” that had arisen.
Meanwhile, the inflammatory process is a common consequence of trauma, which is a surgical operation for the body. And this is completely normal.
Moreover, it is the inflammatory process that is the triggering factor, the initiator of regeneration. Without inflammation, regeneration simply will not begin, because all the basic substances, mediators that control regeneration, are formed as a result of inflammation.
Another thing is that the postoperative inflammatory process must be kept under control. It is necessary to create such conditions so that the alteration and exudation phases take place as quickly as possible, without delays or complications. For this:
– the patient is scheduled for postoperative examinations. They are necessary to monitor the condition of the postoperative wound, since only the doctor can determine whether everything is normal and at what point something went wrong. Post-operative control, as I always emphasize, is for your safety. As long as you are under the supervision of a doctor, nothing bad will happen to you.
- medications are prescribed. Typically, drug therapy in the postoperative period consists of two components, antibacterial and anti-inflammatory. The latter reduces the activity of inflammatory mediators, suppresses a number of its mechanisms, prevents acidosis and disruption of membrane transport - this explains the analgesic activity of some anti-inflammatory drugs. But they are precisely ANTI-INFLAMMATORY, which means they should be taken regardless of the severity of the pain syndrome. It should be noted that any medications must be prescribed individually and reasonably.
– postoperative wound care is prescribed to avoid further infection. The constant ingress of microbes can “suspend” the inflammatory process in the alterative or exudative phase - and no proliferation or “recovery” will occur.
– for the same purpose, a special postoperative regimen is prescribed. Its goal is to create peace for the postoperative wound site, stop the action of inflammatory (phlogogenic) factors and ensure a speedy transition to proliferation.
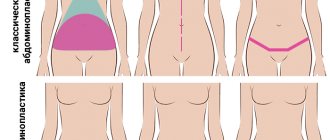
How can you sit after vaginal surgery?
Pose “leg-to-leg” or semi-sideways
Sitting after surgery option 1
Sitting after surgery option 2
You can also use an orthopedic circle or a rubber “vessel”, and the perineum should be in the middle of the circle (in the void), this is especially convenient when driving or while sitting.
You can place 2 stools or chairs next to each other so that the crotch area is in the space between them.
Sitting after surgery option 3
Sitting after surgery option 4
If resection of the labia is performed
Recommended:
- Turnout in 7-10 days.
- Motor and physical activity is strictly prohibited on the first day after surgery; lying on your side is more likely.
- 2 weeks after surgery, it is recommended to perform Kegel exercises (list and technique) to strengthen the vaginal muscles.
- Sexual rest for 1 month.
- Restriction: pool, sauna, bath 2 weeks, shower allowed.
- Limit physical activity for 2 weeks.
- If there is bloody discharge from the genital tract more than 3 sanitary pads per day, increased pain in the lower abdomen, an increase in body temperature above 37.5 degrees, call your doctor by phone: +7-921-311-45-68.
- Treatment with furacillin solution (5 tablets per glass of water) or chlorhexidine solution (aqueous).
- It is mandatory to take broad-spectrum antibacterial drugs; the specific drug is indicated in the discharge certificate.
If hymenoplasty surgery is performed
- Don't sit for 3 days.
- Limit physical activity for 7 days.
- Treatment with furacillin solution (5 tablets per glass of water) or chlorhexidine solution (aqueous).
- If there is bloody discharge from the genital tract more than 3 sanitary pads per day, increased pain in the lower abdomen, an increase in body temperature above 37.5 degrees, call your doctor by phone: +7-921-311-45-68.
- It is mandatory to take broad-spectrum antibacterial drugs; the specific drug is indicated in the discharge certificate.
Alteration
With any trauma-operation, some part of the tissue is inevitably damaged and, to put it mildly, dies. As damaged tissues decay, they release a number of substances that are detected by the body as “Achtung! Kritischer Schaden!” and being, in fact, the initiators of all subsequent reactions. Under the influence of these substances, including lysosomal enzymes, special “kinin” proteins, etc., about 80 types of compounds in total, a number of changes occur in the area of the operation:
– due to the release of enzymes from destroyed cells and disruption of membrane (from/to the cell) transport, the tissue pH changes to the acidic side (acidosis), local buffer systems are inhibited. Developing acidosis is partly the cause of pain in the area of injury and surgery.
– there is an expansion of the “incoming” vessels of the mycocirculatory bed and a narrowing of the “outgoing” ones , plethora occurs, etc. “stasis”, stagnation of blood in the area of trauma-operation. In addition, interstitial pressure increases (again, due to disruption of transmembrane transport mechanisms). This is what explains the swelling, increased temperature and, partly, pain in the area of the operation.
– the permeability of the vascular wall increases, the movement of plasma begins and the release of protective blood cells, leukocytes and lymphocytes, outside the bloodstream.
– under the influence of a number of enzymes (for example, collagenases, ellastases, etc.), the intercellular substance “softens” and swells , which facilitates the movement of protective cells and tissue macrophages in the area of the operation.
– so-called so-called “opsons” are protein marker molecules that indicate what needs to be removed from the body. The attached opsons seem to say to the macrophages “Hey! This is what you need to eat!” This is how the process of phagocytosis begins, discovered and first described by our compatriot, Ilya Mechnikov. For which, by the way, he received the Nobel Prize.
This whole process is called alteration (from Latin - “destruction”), its task is to find and designate what, ultimately, needs to be removed from the body.
We, doctors and you, patients, need to know the following about alteration:
– the start of alteration (and, in general, the inflammatory process) is preceded by a damaging external influence , as a result of which some of the cells lose their viability and die. What matters is the strength and duration of the impact - the larger the area of the operation-trauma, the longer the operation lasts or the traumatic agent affects the body - the more pronounced the postoperative inflammation will be.
– it is the alteration phase that gives us the majority of unpleasant postoperative symptoms , such as pain, swelling, redness, fever, etc. The severity of these symptoms will depend on the intensity of the alterative stage of inflammation.
– at the alteration stage, substances are released that largely determine the entire further course of the inflammatory process and subsequent regeneration. In other words, without destruction there is no creation.
– disruption of the microcirculatory bloodstream, an imbalance between the inflow and outflow of blood, leads to “demarcation” of the inflammation zone - the body, as it were, delimits the site of injury-surgery and prevents the inflammatory process from spreading further. As a result, even a significant local inflammatory process often does not lead to a global disruption of the functioning of the body or the manifestation of any general symptoms - increased body temperature, deterioration of well-being, etc.
In the alterative phase of inflammation, the body prepares the agents that caused inflammation, namely, decay and fragments of dead cells, microbes and damaged fibers of the intercellular substance, for removal from the body. But the very removal of all nasty things occurs in the next phase of the inflammatory process - exudation.