In what cases is nipple areola reduction recommended?
Dr. Philip Nikolaevich Mistakopulo will help eliminate the defect that is bothering you and make your breasts beautiful and attractive. You can adjust your areolas and nipple shape not only after pregnancy and breastfeeding, but also in the following cases:
- enlarged areola as a result of a congenital anomaly - tubular breast;
- congenital asymmetry in size, location or shape;
- acquired asymmetry - as a result of surgery;
- The size of the areolas is too large from a woman’s point of view, causing complexes and discomfort.
Before surgery, you must consult with a surgeon. He will examine the breasts, assess the condition of the tissues, and select the optimal correction method.
increase in nipple halo
You have become the mother of a charming baby. It would seem that all the difficulties are behind us... However, childbirth is a serious test for the body. After them, complications may arise, which, fortunately, in many cases are easy to avoid. The first days you spend with your newborn baby are a happy time. However, it is often overshadowed by various postpartum troubles, which, if left untreated, can cause serious complications. The postpartum period, depending on the individual characteristics of the woman, lasts from six to ten weeks.
During this time, the internal organs and systems of the body, which underwent changes during pregnancy, return to their previous state. And this process, alas, does not always happen easily and painlessly. The main group of complications of the postpartum period are pelvic inflammatory diseases caused by infections of the genitourinary organs of the mother who were not treated during pregnancy. Other reasons for their development are a decrease in the immunity of the new mother and non-compliance with simple rules of intimate hygiene.
PATHOLOGICAL POSTPARTUM BLEEDINGS
In itself, uterine bleeding after childbirth is not a symptom of a pathological process and, until a certain time, is considered a normal phenomenon, absolutely natural for the postpartum period. Over the nine months of pregnancy, the uterus with the baby growing in it significantly increases in size, and at the time of birth its weight, as a rule, is about 1000 grams. Empty after the birth of a child, it contracts, returning to its previous size. During uterine contractions, bloody discharge appears from the vagina, similar to heavy menstruation. These are lochia. Normally, they are abundant, thick and bright red only in the first week after birth. They then fade, become more scanty, and normally stop after six to eight weeks. For mothers who breastfeed their babies, they end earlier. In women who have had a caesarean section, on the contrary, they last a little longer. But there are cases when uterine discharge can be pathological.
HOW DO THEY MANIFEST
A young mother should be wary if lochia two weeks after birth is still abundant, has a rich bloody color, has acquired a strong unpleasant odor, has become purulent, or if after bloody discharge the bloody discharge begins again. All this may be a sign of a developing complication, which will not go away on its own without medical help. Delayed postpartum discharge is no less dangerous for a woman. This indicates a bending of the uterus and a slow rate of contraction. In this case, a woman experiences a sharp decrease in lochia secretion, a feeling of heaviness in the lower abdomen and lower back, chills, and an increase in temperature.
IMPORTANT! The development of postpartum inflammation is caused by: blood loss during childbirth, anemia, vitamin deficiency, blood clotting disorders, remnants of the placenta or membranes in the uterine cavity, surgical intervention during childbirth, severe pregnancy, etc.
PREVENTION
Maintain genital hygiene. During the entire period of bleeding, especially if there are postpartum stitches on the perineum, wash with cool, clean water after each visit to the toilet. Change pads every 4 hours. It is important that the pad, especially in the first 5-7 days after birth, does not fit closely to the vagina: it is necessary to create a ventilation effect.
Inflammation in a woman in labor can be caused by microbes coming either from the vagina, or from foci of chronic infections inside the body. If a woman is at risk for such diseases, she may be placed in a specialized department for childbirth.
- To avoid complications, it is necessary to promptly treat all possible infections, especially gynecological ones.
- Do not use sanitary tampons - this is a sure way to introduce infection into the uterus.
- Lie on your stomach more often in the first week after birth; in this position, the uterus will contract more actively.
- Don't lie around after childbirth. If the birth went without complications and your health allows, start moving as early as possible.
- Empty your bladder and bowels in a timely manner.
POSTPARTUM ENDOMETRITIS
Today, endometritis (inflammation of the mucous membranes of the uterus) is the most common complication that women face during the postpartum period. It occurs in 7% of women in labor, and more often this pathology occurs in mothers who have had a caesarean section. The inner surface of the uterus after the birth of the baby is an extensive wound surface. Its healing includes two stages: inflammation and restoration of the mucous membrane, due to which the inner surface of the uterus is cleansed. However, in the presence of pathogenic microorganisms, the inflammation process can become chronic.
HOW IT MANIFESTS
Endometritis varies in severity. Severe - appears on the second to fourth days after birth, in a mild form - on days 5-12. The woman’s temperature rises to 38°C, chills begin, and her pulse quickens. Pain is felt in the lower abdomen and lumbar region, which intensifies during feeding - it can be dull, insignificant or intense, radiating to the stomach. Discharge from the uterus acquires an unpleasant odor, becomes brown, and later becomes purulent. During a gynecological examination, it is noted that the uterus contracts slowly, the height of its fundus does not correspond to the postpartum period.
It should be noted that a slight increase in temperature (up to 37.5°C) and a feeling of weakness in the first days after birth can be caused by the arrival of milk and is not a sign of the development of an inflammatory process.
REASONS FOR DEVELOPMENT
Endometritis develops due to the penetration of microbes into the uterus. This may happen for the following reasons:
- As a consequence of hormonal or surgical correction in case of threat of miscarriage.
- If a woman has been diagnosed with infectious, including gynecological, diseases during pregnancy.
- After a caesarean section.
- After examinations carried out using an invasive method, that is, with the introduction of medical instruments into the uterine cavity. In particular, amnioscopy (examination of amniotic fluid through the abdominal wall) and amniocentesis (sampling of amniotic fluid).
- During long labor. Especially if more than 12 hours have passed from the moment of rupture of amniotic fluid to the birth of the baby (the so-called “water-free” period).
- In case of complications during childbirth: weakness of labor, application of obstetric forceps, in cases where the placenta is poorly separated and parts of the placental tissue remain in the uterus.
- If the baby was born large or with multiple births, in these cases the uterus is overstretched, so it is difficult for it to contract after childbirth.
- If a woman fails to comply with simple rules of intimate hygiene during the postpartum period.
PREVENTION
- Timely and effective treatment of infectious diseases during pregnancy and complications arising during labor.
- Administration of antibacterial drugs during and after surgery to women at high risk.
- Prophylactic use (exclusively as prescribed by a gynecologist) of antibiotics at a relatively high risk of developing endometritis (for example, after a cesarean section).
- For any ailments during the postpartum period, consult a doctor; do not self-medicate.
- Isolated stay of the mother with the baby in the postpartum ward.
INFLAMMATION OF THE URINARY TRACT
If during the first day after childbirth a woman feels pain and burning when urinating, this is quite normal. But if this discomfort persists after 3-4 days, as well as after healing of tears or cuts in the perineum, this may indicate the onset of infection.
HOW IT MANIFESTS
There are difficulties with urination, pain, or the need for it without urine output (or with little urine output). Urine is usually cloudy in color and has a strong odor. The temperature is elevated, pain is felt in the lumbar region on both sides.
PREVENTION
Drink more fluids. Unsweetened cranberry juice is especially good in this case - it has an antimicrobial effect due to the high concentration of tannin, which does not allow bacteria to attach to the walls of the bladder. But you should avoid black coffee and sweet sodas (if your baby is breastfed, these drinks are prohibited for you).
- Try to empty your bladder every 2 hours in the first days after birth.
- Wash yourself more often, this will stimulate urination.
- After visiting the toilet, when wiping yourself with toilet paper, make movements in the direction from the anus to the back.
- When urinating, try to ensure that the urine comes out completely. To do this, try leaning forward while urinating - in this position, the last drops will come out of the bladder.
REASONS FOR DEVELOPMENT
- Insertion of a catheter during the birth process.
- Bladder injury during natural childbirth.
- Decreased bladder tone, especially after epidural anesthesia.
- Injuries received during childbirth when applying obstetric forceps or a vacuum extractor.
If you have postpartum complications, we recommend that you contact www.kliniki-lechenie.ru, where you can choose a clinic with highly qualified staff and many years of experience in treating postpartum complications.
POSTPARTUM MASTITIS
Only a nursing mother can face such a dangerous disease. Its main causative agent is staphylococcus, which penetrates the breast tissue through cracks in the nipples and through the milk ducts.
HOW IT MANIFESTS
Postpartum mastitis is accompanied by a rise in temperature to 38.5°C and above, chills, weakness, and headache. The mammary glands (or one mammary gland) become painful, the skin in the affected area turns red, the breasts become hot and swell. Upon manual inspection, significant compactions can be felt in it. When breastfeeding a baby or expressing milk, a nursing mother experiences excruciating, acute pain.
The best prevention of such a dangerous postpartum disease as inflammation of the mammary gland, that is, mastitis, is regular expression of milk. It is important to express breast milk completely, to the last drop, because the milk ducts with the drops remaining in them are the most favorable environment for the development of harmful bacteria that cause infections.
REASONS FOR THE APPEARANCE
- Incomplete emptying of one or both mammary glands when feeding the baby.
- Deep and non-healing cracks in the nipples.
- It is equally important to prevent postpartum mastitis to properly attach the baby to the breast - this will ensure good milk flow and painless feeding.
- Untreated lactostasis (stagnation of milk in the mammary glands). It is very important to distinguish lactostasis from mastitis in a timely manner. With lactostasis, expressing milk brings noticeable relief, redness and swelling of the skin are not observed, milk is released freely. After pumping, the body temperature returns to normal and the pain stops.
PREVENTION
- Compliance with the rules of hygiene for breastfeeding a child: cleanliness of mother’s hands and nipples.
- Correct placement of the baby to the breast: he should grasp the nipple and areola.
- Regular pumping (after each breastfeeding) to prevent milk from stagnating in the ducts.
- Timely treatment of cracked nipples and lactostasis.
- Air baths for the breast, lasting 10-15 minutes after feeding.
POSTPARTUM PERITONITIS
Inflammation of the peritoneum, which leads to disruption of all body systems. Most often it occurs as a complication after cesarean section. The state of the mother's immune system, which is weakened by surgery, blood loss, and stress, is also of great importance. With peritonitis, there is a gradual “poisoning” of all body systems with toxins and disruption of their functions. To treat it, complex therapy is carried out: surgical removal of the source of infection, as well as detoxification, that is, the removal of toxins.
HOW IT MANIFESTS
Symptoms appear early - towards the end of the first or at the beginning of the second day after birth. There is an increase in temperature, bloating and pain in the lower part of the abdomen on both sides, nausea, and vomiting. There is often scanty bleeding from the uterus.
REASONS FOR THE APPEARANCE
- Complications after cesarean section, in particular wounds of the anterior abdominal wall.
- An incision in the uterus during a caesarean section, a common consequence of which is burst blood and lymphatic vessels.
- The presence of a suture on the uterus, interfering with its normal contraction and outflow of lochia in the postpartum period.
- Penetration of infection into a broken suture on the uterus after cesarean section.
- Disease of the appendages.
- Development of endometritis in the postoperative period.
- Extragenital diseases of women (appendicitis, damage to the wall of the rectum or bladder).
PREVENTION
- Timely and effective treatment of existing viral infections during pregnancy and after childbirth.
- Staying isolated from other patients in the postpartum ward for mother and baby.
- Prophylactic use (but only as prescribed by an obstetrician-gynecologist) of antibiotics at a high risk of developing an inflammatory process.
- A woman's compliance with all recommendations after a caesarean section.
- Maintaining personal (especially intimate) hygiene.
- BLOODY DISCHARGE from the genital tract in the first 6-8 weeks after birth. As already mentioned, lochia is caused by contraction of the uterus, rapidly returning to its previous size. How to help yourself. Do not forget about intimate hygiene, use pads with a high degree of absorption. You should stop using tampons during this period.
- INVOLUTIONARY URINATION. Occurs due to the absence of the urge to empty due to an increase in the volume of the bladder after childbirth and the presence of free space in the abdominal cavity. In this case, the woman does not feel the urge to urinate. Most often, urinary incontinence occurs when laughing, coughing and sneezing. If incontinence does not go away within three to four months after giving birth, you should consult a doctor.
How to help yourself? Perform daily exercises to strengthen your pelvic floor muscles - Kegel exercises.
- PAINFUL URINATION in the first days after childbirth. It may be due to urine getting onto the stitches from cuts or tears in the perineum. Pain when urinating is also caused by the insertion of a catheter into the urethra during labor.
How to help yourself? Try emptying your bladder while standing, with your legs slightly bent at the knees, so that less urine gets into the damaged areas. Applying cold compresses to the perineum for 30 seconds after each wash will also help.
- CONSTIPATION. After childbirth, the uterus, which has not yet returned to its previous size, puts pressure on the intestines, the motor activity of which is still reduced, the muscles of the abdominal press and perineum are weakened. All this, combined with the psychological stress of a woman who has become a mother, can cause constipation in the postpartum period.
How to help yourself? Actively include fiber-rich foods in your diet. Intestinal function is stimulated by dried apricots, prunes, wholemeal bread, buckwheat, rolled oats, durum wheat pasta, and boiled beets. Drink enough fluids - breastfeeding mothers need at least 2.5 liters per day. And, of course, move more.
- Swelling, heaviness in the chest. Milk comes in approximately 2-4 days after the baby is born. With the appearance of milk, the breasts increase significantly, swell, become heavy, and hot. Touching may be painful. You may feel lumps that disappear after pumping.
How to help yourself? Pump regularly, put your baby to your breast more often, and use creams and ointments that relieve sore nipples.
- GENERAL WEAKNESS. A woman’s body has undergone tremendous hormonal stress during pregnancy, and now it has to get used to the new state. This does not pass without a trace. And besides, the new mother has more worries with the baby. She needs time to recover, regain strength and energy.
How to help yourself? You just need to wait. The body will soon return to normal, because this is provided by nature itself - you need strength to care for the child. Try to get enough sleep at least occasionally, go for a walk, take vitamins, and most importantly, smile more often and, despite all the difficulties, be glad that you are a mother.
KEGEL EXERCISES FOR “INTIMATE” MUSCLES
Perform each of them daily: 5 sets of 10 repetitions.
- Tighten the muscles of the perineum, weakened after childbirth, hold them in this state for 3 seconds, then relax.
- Gently squeeze your perineum muscles for 3-5 seconds, then relax (as in the previous exercise). Then tense your muscles a little harder for a few seconds. After each approach, relax gradually, holding varying degrees of tension for 2-3 seconds.
- Tighten and relax your intimate muscles as quickly as possible. After this, push as if giving birth.
How is nipple correction surgery performed?
Correction of the nipple-areolar complex is performed under local or general anesthesia. The type of anesthesia depends on the complexity of the operation: if the surgeon reduces the areola at the same time as a breast lift, augmentation or reduction, general anesthesia is performed. If you only need to correct the areolas, local anesthesia is sufficient.
To reduce the areola and improve its shape, the surgeon makes an incision along the border of the pigmented area and the skin of the breast. Then he excises the pigmented area, removing excess tissue and creating a beautiful symmetrical shape of the areola. If asymmetry is observed, the surgeon can reposition the nipple-areola complex, achieving an aesthetically pleasing result.
After correction, external cosmetic sutures and special dressings are applied. Due to the fact that the incision is made in the transition area, the surgical sutures are almost invisible. After the rehabilitation period they will become invisible.
Correction of areolas and nipples
Breast lift surgery is often performed with simultaneous correction of the shape of the breast and correction of the nipple-areolar complex.
However, correction of areolas and nipples is often performed as an independent operation. This procedure gives a woman the opportunity to quickly and effectively get rid of imperfections that have bothered her all her life (anomalies in the development of the nipples, sloppy appearance of the areolas, excessive or absent pigmentation of this area, etc.).
Indications for correction of the shape of nipples and areolas:
• retraction or flattening of the nipple;
• excessive nipple protrusion;
• underdevelopment or absence of the nipple;
• violation of the symmetry of areolas and nipples;
• unaesthetic appearance of the areola (disproportionately large or small pigment circle, uneven or dark color).
Manipulations with the nipple-areolar complex can be performed under local or combined anesthesia (if simultaneous intervention, including endoprosthetics or breast lift, is not planned). The operation takes on average about 1 hour.
Important! Since not all methods guarantee unhindered breastfeeding in the future, it is necessary to carefully and comprehensively discuss this issue with the surgeon and assess the risks.
We list the most popular surgeries to correct areolas and nipples:
Correction of nipple shape (nipple reduction). During the operation, excess nipple tissue is excised, then a cosmetic suture is placed on the nipple.
Correction of inverted nipples. The operating doctor makes an incision at the base of the nipple, separates the structures that pull it inward, then secures the nipple in the proper position, preventing it from relapsing.
Reduction of nipple areolas. The surgeon excises excess skin along the edge of the areola, forms the boundaries of the new areola, then applies internal and external (cosmetic) sutures. The areola circumference can be reduced by 3-4 cm.
Enlargement of nipple areolas. This is an aesthetic manipulation used to correct unexpressed, absent or weakly pigmented areolas, as well as their asymmetry. A pigment is injected into a pre-marked area of skin that imitates the natural color of the areolas.
After the operation, the patient also remains in the hospital for some time, then is sent home. For speedy rehabilitation and consolidation of the result, you should wear supportive underwear made of special knitwear and follow the doctor’s instructions.
Breast lift with correction of areolas and nipples. Photos before and after surgery.
1 Photo before breast lift with correction of areolas and nipples
2 Photos after a breast lift with correction of areolas and nipples
3 Photos after a breast lift with correction of areolas and nipples
If you dream of improving something in your appearance, for example, resorting to a breast lift or correction of the nipple-areolar area, make your decision consciously! Study professional medical articles and reviews about breast lift, visit the clinics you like, and personally consult with doctors. Your decision about breast surgery should be balanced!
Be sure to visit the MedicCity multidisciplinary clinic. Our plastic surgeons have impressive practical experience and are proficient in all classical and innovative methods of breast correction!
What you need to know about the rehabilitation period
The rehabilitation time depends on the complexity of the surgical intervention. If plastic surgery is performed under general anesthesia, you will need to spend a day in the clinic under the supervision of a doctor. The very next day you can be discharged and return home.
Primary discomfort: pain, swelling, slight increase in temperature - disappears in 1-3 days. You should not shower or bathe for the first 7-10 days after plastic surgery. Your doctor may recommend special underwear for you. He will schedule dates for suture removal and follow-up examinations.
Areola sizes
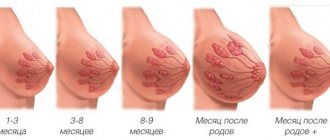
The color and size of the areolas may change over time
Each body is unique and each woman's breasts are unique, so there is no “correct” size for nipples and areolas. A 2009 study in Japan involving 300 adult women found that the average diameter of the participants' areolas was 4 centimeters.
As part of an earlier study, Israeli experts examined the ratio of breast, areola and nipple sizes in 37 women aged 20 to 64 years. Scientists found that on average, areolas were three times the size of nipples.
However, areolas whose dimensions do not fit into such proportions do not indicate health problems. They can also naturally change size and color over time.
The characteristics of a woman's breasts often change due to hormonal changes that occur during puberty, menstruation, pregnancy and breastfeeding.