Why are we writing this article
We have been selling lingerie, clothing and medical products for women post-mastectomy for many years. We have a wealth of experience, product training and advice from specialists in this field. During this time, we studied all the details and the level of discomfort that a woman experiences after going through such an experience.
We know for sure that you can regain your previous level of comfort and achieve the desired quality of life. After breast surgery, you can live your normal life and get the same pleasure from it. And we know how to do it.
We want to share our knowledge. And in this article we will tell you what we can offer:
- rehabilitation means with which you can really feel as healthy as possible and look natural and stylish;
- a wide range that we have been honing over the years - we select the most progressive, comfortable and natural products from the world's best manufacturers: exoprosthetics,
- preventative compression sleeves, underwear with pockets, casual clothing, swimsuits;
- Our consultants will teach you how to use and care for these products. And also take care of yourself - they will talk about a gymnastics program to develop your arm and prevent swelling;
- goods of different price categories - for women with different capabilities; a full package of documents and certificates - so that you can receive compensation from the state for the purchase of special goods.
Skin-sparing mastectomy with simultaneous breast reconstruction
Malygin S.E., Malygin E.N., Sidorov S.V., Kondrashov V.V. Russian Oncology Research Center named after. N.N.Blokhin RAMS, Moscow
Breast cancer is currently the most common malignancy among women, with incidence rates increasing annually [1]. Despite the great popularity of breast-conserving treatment, its use is limited to early stages of breast cancer with a tumor no larger than 3 cm, the absence of clinically positive axillary lymph nodes, the size of the breast, tumor location and a number of other reasons [2]. There is also an increase in the number of local recurrences and often unsatisfactory aesthetic results [3]. Also, the frequency of use of organ-preserving treatment depends on the quality of diagnosis of the early stages of the disease in a particular medical institution. Therefore, the main type of radical intervention for breast cancer is still a modified radical mastectomy as modified by Madden, and a large number of patients who have undergone this surgical intervention experience significant psychological difficulties associated with breast loss [4].
One of the main methods of rehabilitation of this category of patients, especially young people, is breast reconstruction. In the past, surgeons often tried to delay reconstruction so that the results of the reconstruction were compared to an “empty” chest wall after a mastectomy. Many women consider this to be evidence of insufficient efforts in the process of psychological rehabilitation after breast removal [5, 6]. In a comparative study of 83 women who underwent reconstructive surgery and 50 patients without reconstruction, 83% of the first group noted that reconstruction was an important point in recovery from the trauma associated with a diagnosis of breast cancer [7]. In a randomized trial of 64 women with operable breast cancer who were offered immediate or delayed reconstruction (12 months after mastectomy), those in the immediate reconstruction group had more positive body image at 3 months than those in the delayed reconstruction group [8]. ]. Women often do not want to undergo delayed breast cancer surgery because they do not want to become patients again and relive the emotional trauma associated with the initial diagnosis of breast cancer.
Another aspect that has long been common among physicians is the belief that one-stage reconstruction may interfere with the detection of local recurrences. A two-year waiting period has often been justified on the basis that recurrence occurs most often during this time period. However, the incidence of local recurrences after simultaneous reconstruction is the same as after mastectomy without reconstruction [9, 10].
Slavin et al. reported a mean locoregional recurrence rate of 11.7% over a mean follow-up of 5.4 years in a series of 120 patients who underwent autologous reconstruction for stage II and III breast cancer. Moreover, relapses were mainly observed in patients with stage III B [11].
Thus, performing reconstruction simultaneously with radical intervention does not affect the prognosis and course of the disease, while its advantages in the rehabilitation of patients after mastectomy are obvious.
Modern methods of breast reconstruction after radical mastectomy, be it the use of silicone implants or the movement of musculocutaneous flaps, face the difficult task of reshaping the shape and volume of the breast. Despite significant progress in the field of reconstructive plastic surgery, associated with the development of a large number of techniques, this problem, as well as the problem of noticeable scars after reconstruction, creates a need for further improvement of approaches to breast reconstruction after mastectomy.
The evolution of surgical approaches from Halstead's radical mastectomy to breast-conserving operations has allowed us to take a broader look at the problem of surgical treatment and pay attention to surgical interventions that were used mainly for benign diseases of the breast or as a preventive procedure. In this case, the main goal, of course, was to improve the quality of life of patients with breast cancer by optimizing the results of reconstructive plastic interventions.
The issue of preserving breast skin in order to improve reconstruction results has remained unresolved since the beginning of the 20th century. Options for operations in which breast tissue was removed while preserving the skin and nipple-areolar complex in order to prevent the development of cancer in the opposite gland and simultaneous reconstruction began to be developed in 1917, when Bartlett performed the first subcutaneous mastectomy with simultaneous replacement of the removed breast tissue with free adipose tissue [12]. Rice and Strickler in 1951 published their data on the results of subcutaneous mastectomy for benign diseases [13]. This problem is also actively addressed by Freeman [14, 15], who uses endoprostheses for breast reconstruction, Pennisi and Capozzi [16-18], and Woods [19]. All of these surgeons perform the same type of operation, in which relatively thick skin flaps are mobilized, and a disk of breast tissue is left under the nipple-areolar complex to improve its blood supply. The common name for this operation is subcutaneous mastectomy.
Another school of surgeons, represented by Thorek [20], Maliniac [21], Bader [22] and Horton [23], advocated the use of a different technique in which thin flaps were isolated, as in a radical mastectomy, and all tissue under the nipple-areolar was removed. complex, despite the risk of necrosis. This type of surgery is called a total glandular mastectomy.
Both of these techniques were developed to perform preventive operations at a high risk of developing breast cancer and were most often accompanied by reconstruction using both native tissue and silicone endoprostheses.
The effectiveness of subcutaneous mastectomy in removing breast tissue was questioned by Goldman and Goldwyn in 1973 when, after a standard subcutaneous mastectomy technique, residual tissue was found in 83% [24]. Another study conducted in 1991 by Barton et al.[25], which compared the amount of tissue left after a modified radical mastectomy and a total glandular mastectomy using a large number of intraoperative biopsies, resulted in 5% positive biopsies for both types of operations, with an average the amount of breast tissue left is 0.2% of the original volume. The conclusion that was reached was that total glandular mastectomy is an effective procedure for removing breast tissue compared to modified radical mastectomy.
Preservation of the areola and excision of the nipple using the “nipple-coring” technique [26], according to the authors, does not pose a danger, since, in their opinion, the ducts are located only in the nipple. However, a special study conducted in 1993 by Schnitt et al. [27], where the presence of ducts in the areolar zone in postmastectomy specimens was studied, showed that the epithelium of the ducts is located on almost the entire surface of the areola, including its peripheral parts. Thus, to reduce the risk of cancer in this area, it is also necessary to completely remove the nipple-areolar complex followed by its reconstruction.
Taking these data into account, in the early 90s. The first publications appeared, published by several surgeons, which concerned modifications of traditional incisions for modified radical mastectomy in order to improve the results of simultaneous breast reconstruction. In particular, the first work on this topic was published in the journal Plastic & Reconstructive Surgery in 1990 by Toth et al. in the section “Ideas and Innovations” [28]. This paper presented a case of simultaneous reconstruction of both mammary glands for mucinous cancer of the right breast in a patient at risk of developing cancer in the other breast. Due to the fact that the patient's mammary glands were large in combination with severe ptosis, a modified radical mastectomy was performed with reduction plastic incisions and a prophylactic mastectomy on the left with simultaneous reconstruction with a bilateral fully de-epithelialized transverse recto-abdominal (TRAM) flap with good aesthetic result. A year later, the same group of surgeons publishes a report on 17 patients who underwent simultaneous reconstruction using a similar technique, which the author called the “Wise pattern,” using various reconstruction techniques. In this work, the term “skin-sparing mastectomy” was first used, and the principles for performing such surgical interventions were also announced. These principles included: 1) removal of all breast tissue 2) removal of the nipple-areolar complex 3) removal of skin in the projection of the preoperative biopsy 4) the ability to perform axillary lymphadenectomy from the same approach.
Since this report, over the course of 7 years, a large number of papers have been published on the safety of skin preservation during radical mastectomy, in particular assessing the likelihood of local recurrences, as well as solving technical issues of reconstruction in these conditions [29-33]. The general conclusion of these works was a significant advantage of the results obtained in comparison with standard methods.
In 1997, works began to appear devoted to the oncological evaluation of this approach in reconstructive plastic surgery of the breast. Thus, Carlson in 1997 published research materials [34], which compared the incidence of local relapses and postoperative complications in groups of patients who underwent standard radical mastectomy (188 operations, average follow-up period 48.2 months) and skin-sparing mastectomy (327 , average follow-up period 37.5 months) with simultaneous breast reconstruction from 1989 to 1994. Local recurrence of invasive cancer in the standard mastectomy group was 9.5%, and in the skin-sparing mastectomy group it was 4.8%. 45% of patients in the first group did not require intervention on the opposite breast, while in the second group, 65% of patients achieved satisfactory symmetry after the first operation. The percentage of necrosis of skin flaps after mastectomy was also compared. In the first group it was 11.2%, and in the skin-sparing mastectomy group it was 10.7%, i.e. was not significantly different. Unfortunately, the authors do not explain what could be responsible for the almost halving of the number of relapses in a group where the theoretical risk of relapse should be higher.
Hidalgo in 1998 published the results of operations for 4 years with an average follow-up period of 27 months, where they did not note a single local recurrence and also did not note an increase in the number of complications after reconstruction [35]. This highlights a significant improvement in aesthetic results. In this case, the author suggests performing axillary lymph node dissection from a separate access.
Researchers from the MD Anderson Center in 1998 published 5-year results of treatment of patients with stage I-II invasive cancer with simultaneous reconstruction, also dividing patients into two groups according to the type of mastectomy performed with simultaneous reconstruction - with skin preservation (104 patients) and without (27 patients) [36]. The percentage of local relapses was 6.7% and 7.4%, respectively, systemic disease progression was 12.5% versus 25.9% in the standard mastectomy group, relapse-free and overall survival rates in the first group were 88.5% and 80.8 %, and in the second 74.1% and 55.6%. Of course, in this situation one can think about the lack of impartiality of surgeons who chose methods for treating certain patients, when patients with a worse prognosis underwent standard surgical interventions.
However, there is no work that has at least indirectly confirmed the deterioration of disease-free and overall survival of patients who underwent skin-sparing mastectomy with simultaneous breast reconstruction.
In this aspect, the work of Newman [37], devoted to local relapses after operations of this type, also deserves interest. In 372 patients with breast cancer T1, T2, for the period from 1986 to 1993, relapses were noted in 23 patients (6.2%) with an average period of appearance of 25 months and in 96% of cases it was represented by palpable formations in the skin of the breast . In 14 patients, the recurrence was treated with surgical excision in combination with systemic therapy. Resection of the reconstructed gland was performed in three patients. Complete local control was achieved in 74% of patients. Nine (39%) developed distant metastases. With a mean follow-up of 26 months, 14 of 23 patients (61%) are alive without signs of disease, 7 (30%) have died.
The authors conclude that the percentage of local recurrences does not differ from the data for recurrence after standard mastectomy, however, these data make us think about the impact of local recurrences on overall survival in this category of patients. In this regard, the approach to treating relapses should be the same as for relapses after modified radical mastectomy.
In light of this information, the next stage of the discussion, apparently, should be the question of the advisability of adjuvant radiation therapy in this category of patients, taking into account the decrease in the aesthetic value of the proposed technique.
Another interesting work on this topic was published in 1998 by Slavin and colleagues [38]. In addition to discussing the technical features of performing mastectomy with skin-sparing and simultaneous reconstruction with a flap on the latissimus dorsi muscle with endoprosthetics, the authors also conducted a study of the presence of the epithelium of extra-lobular ducts in the border of breast skin resection at a distance of 5 mm from the areola. In none of the 144 biopsies from 32 patients were ductal epithelial cells found. The local recurrence rate was 2% with a mean follow-up of 45 months.
At the N.N. Blokhin Russian Cancer Research Center of the Russian Academy of Medical Sciences, skin-sparing mastectomy has been performed in the surgical department of reconstructive treatment since 1995. Currently, the data from this department, the III Oncology Department of the city clinical hospital No. 1 in Novosibirsk, and the general oncology department of the regional clinical hospital in Tula have been combined. In total, by February 2000, 58 operations were performed, 23 of them using silicone expanders, in 35 reconstruction was performed with a TRAM flap on a muscular pedicle.
In this case, various types of incisions on the mammary gland were used depending on the location of the tumor, its size and the size and shape of the mammary gland (Figure 1).
Figure 1. Most common breast incisions for skin-sparing mastectomy.
Skin-sparing mastectomy with simultaneous reconstruction was performed in patients with T1-2N0-1M0 breast cancer, with patients with stages IIA and IIB representing the majority. Reconstruction has also been performed in a limited number of patients with stage III breast cancer in whom neoadjuvant chemotherapy was associated with significant clinical benefit. To ensure the reliability of the data obtained, stage III patients were excluded from the study, as well as patients whose follow-up period was less than 6 months. The follow-up period ranged from 7 to 52 months and averaged 25.8 months. Almost all patients received combined and complex treatment; the majority received anthracycline-containing neoadjuvant polychemotherapy (Table 1).
Table 1. Characteristics of clinical observations
| NUMBER OF PATIENTS | 49 |
| STAGES OF BC | T1-2N0-1M0 |
| ONLY SURGICAL TREATMENT | 2 |
| SURGICAL + PCT | 19 |
| L/T+SURGICAL+PCT | 8 |
| NEOADJUVANT PCT (2 OF THEM + L/T) | 20 |
| AVERAGE FOLLOW-UP PERIOD | 25.8 months |
| TERMS OF OBSERVATION | 7 – 52 months |
| LOCAL RECURRENCE | 1 (2%) |
| CANCER IN ANOTHER GLAND | 1(2%) |
| DISTANT METASTASES | 7 (14,2%) |
| PATIENTS DIED | 1(2%) |
The median overall survival rate during follow-up was not reached in this group. During the entire observation period, one patient died from the disease. The two-year actuarial disease-free survival rate was 86.8%, taking into account the fact that the only local relapse was detected during examination of a patient with metastases in the spine. (Figure 2).
Figure 2. Ultrasound picture of breast cancer recurrence in the reconstruction area (the dotted line marks the endoprosthesis border).
We considered it necessary to divide the complications into two groups according to reconstruction methods. Thus, in the reconstruction group using silicone expanders, the total number of complications was significant and amounted to 34.7% and was mainly represented by seroma in the reconstruction area with subsequent infection. At the same time, complications resulting in the removal of the expander amounted to 21.7%. We attribute such a high percentage of complications to insufficient drainage of the musculocutaneous pocket of the expander when the area of the wound surface increases, as well as aseptically unfavorable conditions in the operating room and early postoperative period. The percentage of overall complications in TRAM flap reconstruction that resulted in poor aesthetic results was 14.2%, including late complications such as anterior abdominal wall prolapse. These indicators certainly show the advantage of using the TRAM flap in patients after mastectomy with skin sparing, since an implant made from native tissue has a significant advantage over a synthetic one in conditions of an increased risk of insufficient blood supply to the preserved breast skin. In this case, it is necessary to take into account the consequences of complications, when during reconstruction with silicone expanders, most complications were fatal to the results of reconstruction, i.e. The expander had to be removed when minor seromas or skin necrosis during reconstruction with the TRAM flap did not have a significant impact on the aesthetic results of the reconstructive intervention.
In most cases, we obtained a significant improvement in aesthetic results compared to modified radical mastectomy with simultaneous breast reconstruction.
The main advantages of the proposed approaches to breast reconstruction were that while preserving the breast skin, and primarily in the area of the inframammary fold, the natural boundaries of the breast were preserved, which greatly facilitated the modeling of the reconstructed gland (Figure 3) When using TRAM - flap, in several cases we performed simultaneous reconstruction of the nipple, thereby relieving the patient of the need for repeated reconstructive intervention; intradermal tattooing of the areola was performed on an outpatient basis (Figure 4).
Figure 3 A, B - View of the patient after mastectomy with skin sparing, reconstruction with TRAM flap and reconstruction of the nipple and areola
Figure 4. Patient, 49 years old. Right breast cancer T2N0M0.
(A) Preoperative marking (B) View after mastectomy with skin sparing and breast reconstruction with a TRAM flap, reconstruction and tattooing of the nipple-areolar complex and endoprosthetics of the left breast
The need for surgery on the contralateral breast has significantly decreased due to the achievement of adequate symmetry after the first stage of reconstruction (Figure 5)
Figure 5 A, B — View of the patient after mastectomy with skin sparing and reconstruction with TRAM flap
Of high aesthetic value is the absence of rough scars in the décolleté area, as well as the absence of contrast between the skin of the chest wall and the skin of the flap, which inevitably accompany reconstruction after a modified radical mastectomy (Figure 6).
Figure 6. Patient, 42 years old. Left breast cancer T1N0M0. (A) Preoperative marking (B) View after skin-sparing mastectomy and simultaneous TRAM flap reconstruction, nipple and areola reconstruction, and areola tattoo.
The problem of noticeable scars on the anterior abdominal wall after previous surgical interventions was resolved. When using the TRAM flap after radical mastectomy, these scars moved into the reconstruction area and significantly reduced the aesthetic value of the reconstructive operation. When saving breast skin flaps, it was always possible to cover scars with them (Figure 7).
Figure 7. Patient, 43 years old. Right breast cancer T2N1M0. Condition after 4 courses of polychemotherapy. There is a history of lower median laparotomy for surgical delivery.
(A) Preoperative view (B) Deepithelialization of the flap with a transverse scar. (B) View after skin-sparing mastectomy with TRAM flap breast reconstruction and simultaneous nipple reconstruction.
In the case of the use of tissue expanders, especially anatomically shaped ones, it was also possible to improve the shape of the reconstructed breast due to the preservation of the inframammary fold (Figure 8), although the high rate of complications indicates the need to improve surgical techniques and approaches to postoperative management of this group of patients.
Figure 8. Patient, 39 years old. Right breast cancer T2N1M0. Condition after 4 courses of polychemotherapy.
(A) Preoperative marking. (B) View after skin-sparing mastectomy and implantation of a tissue expander (C) View on the operating table after replacing the expander with an endoprosthesis, nipple reconstruction and endoprosthetics of the left breast
Taking these data into account, of course, one should recognize the promise of surgical interventions of this type for early breast cancer in conditions where organ-preserving treatment cannot be carried out for oncological indications or due to unsatisfactory aesthetic results, and radical mastectomy, despite its reliability, creates a large number of additional problems.
The emergence of the possibility of performing reconstructive operations with such results not only contributes to the popularization of breast reconstruction among surgeons and patients, but also creates the need to improve surgical techniques and master the methods of reconstructive plastic surgery by oncologist surgeons.
Of course, long-term results still need to be assessed, but preliminary data convincingly prove the validity of such approaches to the problem of rehabilitation of patients with breast cancer.
BIBLIOGRAPHY
1. Trapeznikov N.N., Aksel E.M., Barmina N.M. The state of oncological care to the population of the CIS in 1996. M. 1996 p. 19-24).
2. Kubli F., Fournier Dv Breast diseases. 1989 Heidelberg:Springer-Verlag 209-217.
3. Hayward CZ Breast conservation. J Clin Oncol 1990 6:763-772.
4. Stevens L, McGrath M, Druss R, Kister S, Gump F and Forde K, The psychological impact of immediate breast reconstruction. Plastic and Reconstructive Surgery 1984;73:619-626.
5. Noone RB, Frazier TG, Hayward CZ, et al: Patient acceptance of immediate reconstruction following mastectomy. Plast Reconstr Surg 69:632-638, 1982.
6. Wellisch DK, Schain WS, Noone BR, et al: Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg 76:713-718, 1984.
7. Rowland JH, Holland JC, Chaglassian T, et al: Psychological response to breast reconstruction: Expectations for and impact on postmastectomy functioning. Psychosomatics 34:241-250, 1993.
8. Dean C, Chetty U, Forrest A, Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. The Lancet 1983;459:462.
9. Kroll SS, Ames F, Singletary SE, et al: The oncologic risks of skin preservation at mastectomy when combined with immediate reconstruction of the breast. Surg Gynecol Obstet 172:17-20, 1991.
10. Johnson CH, Van Heerden JA, Donohue JH, et al: Oncological aspects of immediate breast reconstruction following mastectomy for malignancy. Arch Surg 124:819-824, 1989.
11. Slavin SA, Love SM, Goldwyn RM: Recurrent breast cancer following immediate reconstruction with myocutaneous flaps. Plast Reconstr Surg 93:1191-1204, 1994.
12. Bartlett W. An anatomical substitute for the female breast. Ann Surg 1917 66:208–211.
13. Rice CO, Strickler JH Adenomammectomy for benign breast lesions. Surg. Gynecol. Obstet. 1951 93: 759.
14. Freeman BS Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast. Reconstr. Surg. 1962 30:676.
15. Freeman BS Technique of subcutaneous mastectomy with replacement: Immediate and delayed. Br. J. Plast. Surg. 1969 22:161.
16. Pennisi VR, Capozzi A. The incidence of obscure carcinoma in subcutaneous mastectomy: Results of a national survey. Plast. Reconstr. Surg. 1975 56:9.
17. Pennisi, VR Subcutaneous mastectomy and fibrocystic disease of the breast. Clin. Plast. Surg. 1976 3: 205.
18. Pennisi VR, Capozzi A. Subcutaneous mastectomy: An interim report on 1244 patients. Ann. Plast. Surg. 1984 12: 340,.
19. Woods JE Subcutaneous mastectomy: Current state of the art. Ann. Plast. Surg. 1983 11:541.
20. Thorek M. Plastic Surgery of the Breast and Abdominal Wall. Springfield, Ill.: Charles C. Thomas, 1942.
21. Maliniac JW Use of pedicle dermo-fat flap in mammaplasty. Plast. Reconstr. Surg. 1953 12: 110.
22. Bader K., Pellettiere E., Curtin JW Definitive surgical therapy for the “premalignant” or equivocal breast lesion. Plast. Reconstr. Surg. 1970 46:120.
23. Horton CE, Carraway JH Total Mastectomy with Immediate Reconstruction for Premalignant Disease. In R. M. Goldwyn (Ed.), Plastic and Reconstructive Surgery of the Breast. Boston: Little, Brown, 1976. Pp. 459-464.
24. Goldman LD, Goldwyn RM Some anatomical consideration of subcutaneous mastectomy. Plast. Reconstr. Surg. 1973 51:501.
25. Barton F., Jr., English JM, Kingsley W., Fietz M. Glandular excision in a total glandular mastectomy and modified radical mastectomy: a comparison. Plast. Reconstr. Surg. 1991, Vol. 88, No. 3, pp. 389-392.
26. Randall P., Dabb R., Loc N. “Apple coring” the nipple in subcutaneous mastectomy. Plast. Reconstr. Surg. 1979 64:800.
27. Schnitt S., Goldwyn R., Slavin S. Mammary ducts in the areola: Implications for patients undergoing reconstructive surgery of the breast. Plast. Reconstr. Surg. 1993 92: 1290.
28. Toth BA, Glafkides MC Immediate breast reconstruction with deepithelialized TRAM flaps: Techniques for improving breast reconstruction. Plast. Reconstr. Surg. 85:967, 1990
29. Kroll SS, Ames F, Singletary SE, et al: The oncologic risks of skin preservation at mastectomy when combined with immediate reconstruction of the breast. Surg Gynecol Obstet 172:17-20, 1991.
30. Elliott, L.F., Eskenazi, L., Beagle, P.H., Jr. et al. Immediate TRAM flap breast reconstruction: 128 consecutive cases. Plast. Reconstr. Surg. 92:217, 1993.
31. Dinner, M. I., Sampliner, J., Artz, J. S., et al. Optimal cosmetic autogenous reconstruction with modified radical mastectomy. Surg. Gynecol. Obstet. 176:83, 1993
32. Bensimon, RH, Bergmeyer, JM Improved aesthetics in breast reconstruction: Modified mastectomy incision and immediate autologous tissue reconstruction. Ann. Plast. Surg. 34:229, 1995
33. Malygin E.N., Malygin S.E. A new technique for performing primary breast surgery using a recto-abdominal flap for cancer. All-Russian conference “Reconstructive and restorative surgery of the breast” Moscow September 1996. Conference materials pp. 78-79
34. Carlson GW, Bostwick J. Jr., Styblo TM, Moore B., Bried JT, Murray DR, Wood WC Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann.Surg., 225:570-5 1997
35. Hidalgo DA Aesthetic refinement in breast reconstruction: complete skin-sparing mastectomy with autogenous tissue tissue. Plast. Reconstr. Surg. 102:63-70 1998
36. Kroll, SS, Schusterman, MA., Tadjalli HE, Singletary SE, Ames F. Risk of recurrence after treatment of early cancer with skin-sparing mastectomy. Ann. Surg. Oncol. 4:193-7 1997
37. Newman LA, Kuerer HM, Hunt KK Kroll, SS, Ames F., Ross MI, Feig BW, Singletary SE Presentation, treatment, and outcome of local recurrence after skin-sparing mastectomy and immediate breast reconstruction. Ann. Surg. Oncol. 5:620-6
38. Slavin SA, Schnitt SJ, Duda RB, Houlihan MJ, Koufman CN, Morris DJ, Troyan SL, Goldwyn RM Skin-sparing mastectomy and immediate reconstruction: oncologic risk and aesthetic results in patients with early-stage breast cancer. Plast. Reconstr. Surg. 102:49-62, 1998
AUTHORS:
Malygin Evgeniy Nikitich - Doctor of Medical Sciences, Professor, Head of the Surgical Department of Rehabilitation Treatment of the Russian Oncological Research Center named after. N.N. Blokhin RAMS. 115478 Moscow Kashirskoe highway, 24 department of rehabilitation treatment of the Russian Cancer Research Center RAMS tel. 324-90-44
Sidorov Sergey Vasilievich - Doctor of Medical Sciences, Professor, Head of the 3rd Oncology Department of the Municipal Clinical Hospital No. 1 of Novosibirsk, Chief Oncologist of the Ultrasound Health Department of the Novosibirsk City Hall. 630047 Novosibirsk st. Zalesskogo, 6 tel. Municipal Clinical Hospital No. 1 of Novosibirsk.
Kondrashov Vladimir Vladimirovich - oncologist of the department of general oncology of the regional clinical hospital of Tula 300010 Tula, 38 Williams St., apt. 83 tel. (0872) 487-069
Malygin Sergey Evgenievich - candidate of medical sciences, assistant at the department of oncology of the Russian State Medical University. [email protected] 115446 Moscow st.
Academician Millionshchikova, 18 kv. 411 tel. 324-63-53 e-mail (Visited 247 times, 1 visits today)
About experiences and complications
The most important thing is behind us - the operation is done. Life saved.
But the feeling of anxiety continues to live. Now for other reasons.
How now, after the operation, will people around you perceive your body? After all, you want to be beautiful and be liked - in the mirror, by the man you love, to be on an equal footing with your friends. I want to live my life as before, and not have anything overshadow the joy of simple things. Just relax and feel as attractive as before. Realize that everything is okay.
And as soon as all these normal desires are formed, embarrassment and confusion immediately appear. Self-confidence as a woman quickly declines. Sadness takes its place.
Yes, there are tasks that can become reality and for which you need to remain fully prepared:
- physical features: lymphedema, uneven suture, partial resection, stiffness, sweating, weight change, spinal problems;
- psychological state: sadness and confusion about what and how to do next.
And here we want to draw attention to the recommendations and products we offer. Because they are designed specifically to restore a woman’s previous comfort and maintain her health.
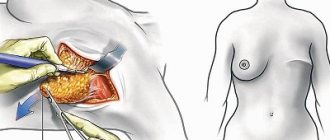
TRAM flap reconstruction method
Reconstruction with a TRAM flap (transverse rectus abdominis myocutaneous flap) of the breast is performed using donor tissue taken from the area in the lower abdomen.
A kind of tunnel is made under the patient’s skin, running from the donor area (in this case, the lower abdomen) to the restored area. Donor tissue includes a skin flap, a fat layer and part of the muscle tissue.
The borrowed piece of tissue is transferred on a so-called vascular pedicle, that is, it will subsequently receive a direct blood supply.
Advantages of TRAM flap reconstruction:
— There is no risk of allergies to your own tissues; — The consistency and temperature of the future breast will be as close as possible to natural; — Additionally, the patient receives abdominoplasty (tummy tuck).
Disadvantages of TRAM flap reconstruction:
— Scar in the lower abdomen; — There must be sufficient fatty tissue in the lower abdomen; — The risk of a hernia in the abdominal area increases, as well as weakening of the abdominal muscles; — The operation is quite traumatic and extensive; it can take from three to eight hours.
More information about TRAM flap reconstruction:
Breast reconstruction using a TRAM flap can be performed on a vascular pedicle (when the donor site continues to receive nutrition from the abdominal area) or can be free. With free movement, the vessels of the donor zone are connected to the vessels in the chest area using a microsurgical method. Reconstruction with a TRAM flap is performed when the patient needs to restore part of the pectoral muscle lost after a mastectomy. If muscle loss in the chest area is relatively low, another DIEP flap technique can be performed.
Postoperative period: what to buy
For the first time after surgery, two products are needed. This is a post-operative prosthesis and bra. In the article we will talk about the best samples - with excellent production quality and high wear resistance.
1. During the postoperative period, doctors advise wearing a primary textile prosthesis. It solves the following problems:
- compensates for volume;
- does not interfere with the healing of sutures;
- protects the skin;
- does not put pressure on the postoperative surface, it can be worn two to three weeks after surgery, until the drainage and bandage are removed;
- The woman individually adjusts the volume of the prosthesis herself.
The prosthesis is suitable for any breast and is adapted for any type of operation:
- radical mastectomy;
- radiation therapy;
- partial resection.
It is used as an overlay for asymmetry and regulates and corrects volume as weight changes.
Perfectly imitates the shape of the breast, due to the compacted molded part of the prosthesis, even if you remove all the filler, the shape of the prosthesis will not change. The product is securely fixed in the bra.
This prosthesis is multifunctional. In the future, it can be used at home - for unloading and replenishing volume. You can sleep, work, and move actively in it. Wearing a primary prosthesis has no contraindications or restrictions. No precautions are required when transporting in travel bags or suitcases. And alternating a silicone prosthesis with a textile prosthesis extends the service life of both products.
2. The second product is a post-operative bra
This product takes into account all the features of the postoperative period. Made from cotton - soft and breathable. And easy to use.
Cups:
- elastic, easily take the shape of both the breast and the postoperative prosthesis;
- The neckline and armhole line are high - the lymph flow is not compressed, postoperative sutures are not visible.
Straps:
- wide, comfortable, softly padded, does not press through the shoulders;
- They do not have length regulators - the strap is elastic and automatically selects the fit on the woman’s back.
Back:
- high, wide, has no fastener;
- allows you to sleep and relax in the bra.
Front clasp:
- comfortable for a woman immediately after surgery - you can put on and take off the bra without assistance;
- With just two buttons and a Velcro fastener, the volume under the bust can be individually adjusted.
In the future, such a bra will be indispensable in the wardrobe for unloading, sleeping and relaxing.
General ideas about reconstructive operations
There are two fundamentally different approaches to breast reconstruction after mastectomy:
- Simultaneous mammoplasty: reconstruction can be done during the same procedure during which the tumor was removed;
- Delayed breast reconstruction: some time after the mastectomy, a repeat operation is performed.
Simultaneous reconstruction is preferable.
- psychological trauma is less pronounced;
- there are no scar tissue changes;
- during a mastectomy, it is possible to preserve the skin and fold under the gland, which gives a better cosmetic result;
- shorter hospital stay;
- no re-operation required.
For breast reconstruction the following are used:
- the patient's own tissue;
- artificial materials (breast silicone implant or expander);
- combination of tissue flap and implant.
The main thing that they try to achieve when restoring the mammary gland is its symmetry with the opposite one. Sometimes this requires surgery on the healthy breast, changing its size and shape.
Constant wearing: what to buy
There are four types of products that you will need to create daily comfort in your everyday life.
1. Clothes
Blouses, T-shirts, pajamas, shirts, dresses, tops, sports T-shirts - these products are designed to be worn without a bra because they have a built-in - sewn-in bodice with pockets to support and secure the prosthesis.
2. Bras
The underwear is tailored in such a way that, thanks to the high neckline, a complete fit of the prosthesis is ensured, scars and uneven postoperative surfaces are hidden. Cups with pockets are responsible for reliable fixation and correct anatomical placement of the breast and prosthesis in the bra, without direct contact of the prosthesis with the body. Wide, ergonomic straps guarantee the prevention of lymphedema and relieve stress from the neck and shoulders - with a heavy bust. The high armhole hides tissue deficiency in the armpit area and provides wearing comfort. The wide belt under the chest does not put pressure on the diaphragm, ensuring free breathing and eliminating discomfort in the stomach area.
3. Swimwear
Swimsuits are tailored like bras, have a stylish appearance, and can be either separate or one-piece.
4. Dentures for permanent wear for an attractive appearance
Modern prosthetics provide natural sensations and behavior. They are soft to the touch, sway when walking and “fall off” when lying down. Designed with a special thin edge - it provides a delicate fit in the sensitive seam area and a natural transition to the lines of the body.
These products are made taking into account the various features of the female breast: full-bodied and lightweight, triangular and teardrop-shaped. They also minimally touch the body, so they do not overheat it - there is no increased sweating, and a natural microclimate is maintained.
Combination of autologous reconstruction techniques and the use of implants
Sometimes there is a need to combine these two reconstruction techniques. In such situations, for example, an implant with the back muscle (latissimus dorsi) and skin are involved in creating the breast.
Nipple and areola reconstruction
Reduction of the right breast in order to achieve symmetry with the left reconstructed breast.
Once the breast contour has been restored, many women choose to have the nipple and areola reconstructed. As a rule, this happens in the long term. There are many techniques for nipple and areola restoration. Most of them are based on the use of local breast tissue, creating a small elevation approximately the same size as the opposite nipple. The areola is reproduced using a tattoo - skin coloring, which is performed in the treatment room.
Opposite (non-removed) breast
The slight difference between the non-removed and reconstructed breasts is not a concern for many women when wearing a bra. For others, the difference in the size of the mammary glands can be quite noticeable, which does not satisfy them. Therefore, some women decide to surgically reduce their unremoved breasts or undergo mastopexy, an operation in which the breasts are raised. For those whose remaining mammary gland is smaller in size than the reconstructed one, it is proposed to enlarge and elevate the unremoved mammary gland.
Beneficial physical activity
Rules for caring for your health:
1. Swimming. Water soothes, has a gentle massaging effect, and the hand recovers faster. Lymph outflow is normalized. The swelling subsides.
2. Exercise. Simple to do but very effective. They will easily become a daily habit.
- “Combing your hair” Place your elbow on the edge of your bedside table. Keep your head straight. Start by combing one half of your head, then gradually move to the other. Don't get overwhelmed, but be persistent;
- “Ball” Clenching and unclenching the hand. Use a rubber ball or other object, squeezing it in your palm;
- “Drying your back” Using a towel or similar object, make gentle movements that simulate drying your back. Repeat on both sides.
3. Wearing a compression sleeve. It is necessary to prevent the occurrence of edema and the threat of lymphedema. Therefore, it needs to be worn under load: work in the country, household chores, flights or a long road. If you couldn’t put on a sleeve during physical activity, be sure to put it on afterwards. Agree that it is better to wear a prophylactic sleeve during exercise than to constantly wear a therapeutic compression sleeve if lymphedema begins to develop.
Recovery after breast reconstruction surgery
An elastic bandage or support bra will help minimize swelling and support the reconstructed breasts.
A small, thin tube may be temporarily placed under the skin to drain excess blood or fluid. Discharge from clinics in St. Petersburg and Veliky Novgorod is carried out on days 3-5, but you can begin a full daily life only after a few weeks. Physical activity, swimming and sun exposure are canceled during this period. The stitches are removed after 7-12 days at the next examination by a doctor. The final results of the reconstruction can be seen after 2-3 months of rehabilitation. Make an appointment: Ask a question!