Langer's lines are conditional lines on the surface of the skin, indicating the direction of its maximum extensibility. They are named after the German anatomist, who in 1861 studied in detail the elastic properties of human skin (article “On the anatomy and physiology of the skin. On the splitting of the skin”).
description
They are round or ribbon-like, straight or crimped fibers of the connective tissue of the skin. If their number increases in a certain place, then they are connected to each other by branches in the form of a network, which easily stretches in the direction of the fibers, and then takes on its original appearance.
Langer's research also showed that the plexus of connective tissue fibers is a lattice-like formation of vascular bundles with loops elongated diagonally. The narrower the loops, the more parallel the vascular bundles are located. According to Langer, the direction of movement of the elastic fibers of the skin is constant and varies in different areas of the body.
The significance of Langer's lines in forensic medicine
Langer lines and skin strength
The strength properties of the skin depend on the direction of the acting force relative to the orientation of the collagen fibers (Langer's lines). The skin provides maximum resistance when the direction of impact coincides with the orientation of these fibers; the specific tensile strength of the skin along the Langer lines requires a load almost 3 times greater than in the transverse direction.
The magnitude of the maximum load leading to skin rupture
Changing the shape of damage
The shape of wounds on the skin, after removing the wounding object, changes its shape. For example, wounds from piercing objects with a ribless surface are not round, but slit-shaped, and their longitudinal dimensions in certain parts of the body are parallel.
There is no dependence of changes in the size of the skin preparation after exposure to fixing solutions relative to the location of Langer's lines.
Skin: functions and structure.
Now we will turn a little to biology, and consider the skin as a living organism. The artist is used to working on canvas, and since a makeup artist is a makeup artist, his main work surface is human skin, which in terms of scale is the largest organ, the area of which in an adult individual sometimes varies from 1.5 m² to 2. 3 m², and makes up approximately 15% of the total body weight. One of its main functions is protective: to protect the body from exposure to the external environment, free radicals, ultraviolet rays, and damage to internal organs. It provides external breathing, participates in thermoregulation, metabolic and excretory processes of the body. Like fabric - it is elastic, porous, durable, waterproof, antibacterial, sensitive. At low temperatures (cold), the lumens of the skin blood vessels are reduced, which means less heat transfer and more heat retention. When the temperature rises, the pores and blood vessels expand, then metabolic processes proceed faster and more intensely, sweating increases and the skin loses a lot of moisture. But do not forget that the intensity of heat transfer will also depend on the humidity of the air (climate), and the thickness of the subcutaneous tissue (including racial characteristics). We have looked at the main functions of the skin, now let's look at its structure. The skin consists of three layers: the outer - epidermis, the middle - the skin itself, or dermis, and the inner - subcutaneous fatty tissue. Each layer performs its own functions. The task of the makeup artist will be to work with the uppermost layer of the skin - the epidermis, since decorative cosmetics are designed for external use and should not affect the lower layers of the skin. Now we will touch in more detail on the structure of the epidermis and working with it, and only superficially then we will touch on the features of the functions and structure of other layers. The epidermis has a thickness of 0.07-2.5 mm. In appearance it resembles a narrow strip, although in fact it consists of 5 layers: horny, shiny, granular, spinous and basal (germ). The last layer contains such an important pigment as melanin. The upper layers of the epidermis become keratinized, forming the keratin (horny) layer, and in its lower basal (germ) layer, on the contrary, cells are constantly formed. Dead cells serve as a protective surface, but they constantly die and slough off, being replaced by new ones. The journey of a new cell from the basal layer to the keratin layer lasts approximately 2-4 weeks. In childhood, cell renewal occurs faster, due to the fact that the body grows; with age, this reproduction speed gradually fades away; visible aging processes begin to appear when the number of dead cells exceeds the number of new ones. Therefore, it is very important to take good care of your skin, cleanse, exfoliate, tone and moisturize it at least 2-3 times a day. In the morning, to put it in order after sleep and metabolic processes, because the body does not stop working when our consciousness turns off. For lunch, for those who have problem skin and well-developed subcutaneous tissue. This requires additional toning and fat removal. In the evening, since during the day it is exposed to external factors (sun, dust, environment), it sweats, removes metabolic products, thereby becoming polluted. Also, before applying decorative cosmetics to the skin, it must be cleaned of cells that have already been exfoliated during the day (with cleansing preparations or tonic), so that cosmetics can then be applied to clean, smooth and even skin. After all, the quality and cleanliness of the work will depend on the condition of the skin. There is even a saying: there is no better makeup than clean and well-groomed skin. Let's return to the epidermis: its deep layers contain pigment cells. They produce the pigment melanin, which affects hair color and skin color in this case, as well as the acquisition of one or another shade of tan. Melanins absorb ultraviolet rays, and thereby protect the tissues of the deep layers of the skin from radiation exposure, deactivate free radicals, and are a catalyst for many biochemical processes. Thus, it is an integral part of the body's immune system. For a makeup artist, the level of melanin determines the level of contrast a person has and their facial tone. The more melanin the skin contains, the darker it is. The largest amount of it is found in the skin of the Negroid race, Indians, Indonesians, etc. Most peoples who live in the equatorial and subequatorial zones, with equatorial and tropical climates, have a high percentage of melanin in their skin; as a result, dark and dark skin serves as protection from intense ultraviolet radiation. Slightly less melanin pigment is found in peoples living in the subtropical zone, with a Mediterranean and subtropical climate: Latin, Eastern, Asian peoples. The average melanin content can be conditionally attributed to people living in a continental climate. And the smallest percentage of pigment will be contained in the skin of people living in the subpolar and polar zones, i.e. among northern peoples, low pigment content also developed historically, due to low-intensity solar radiation, and simply the lack of need for protection from it. And due to the cold and reduction of the lumens of blood vessels, it will appear even lighter, bluer and thinner. The epidermis is practically impermeable to water and solutions based on it. Fat-soluble substances penetrate the epidermis better due to the fact that cell membranes contain a large amount of fat and these substances seem to “dissolve” in the cell membranes. Therefore, many preparations contain emulsifiers that “combine” the water and fat bases. There are also no blood vessels in the epidermis, and its nutrition occurs due to the diffusion of tissue fluid from the underlying layer of the dermis. The next layer of cells is the dermis, or skin itself. This is the inner layer of skin, which has a thickness of 0.5 to 5 mm. It consists of two layers: papillary and reticular. The reticular layer consists of loose connective tissue, which includes the extracellular matrix and cellular elements. The reticular layer consists of loose connective tissue, which includes the extracellular matrix and cellular elements. The basis of cells in the dermis is fibroplast, which synthesizes the extracellular matrix, including collagen, hyaluronic acid and elastin. The dermis contains hair follicles, a large number of blood and lymphatic vessels that provide nutrition to the skin, also participates in heat exchange, it contains pain and sensory nerves, as well as receptors (which branch into all layers of the skin and are responsible for its sensitivity). The excretory function in it is performed by sweat and sebaceous glands. The sebaceous glands secrete fat, which lubricates the hair and skin and makes it elastic, protects the skin from exposure to the external environment, makes the skin waterproof, bactericidal (sebum, together with sweat, creates an acidic environment on the surface of the skin, which has an adverse effect on microorganisms). Sweat glands participate in heat exchange, remove waste products such as water (in the form of sweat), thereby maintaining a constant body temperature, cooling it and preventing it from overheating.
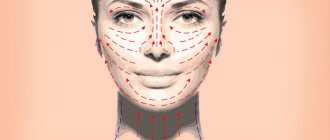
Now we will look at the structural features of the extracellular matrix, which is synthesized by fibroblast, as well as its functions. The absorption of the extracellular matrix includes two main components: the fibrillar part and the matrix. The fibrillar part is the fibers of collagen, elastin, and reticulin that create the framework of the skin. Intertwined with each other, collagen fibers form a network that is located almost on the surface of the skin under the epidermis. This is the framework that gives the skin its strength. In the facial area, collagen fibers create a special dense network, which is strictly laid and ordered so that it forms lines of least stretch - Langer's lines, also known as massage lines. It is along these lines that massage is performed and cosmetics are applied so as not to stretch the skin and not provoke the formation of wrinkles (this massage is best performed with the weakest fingers - the ring fingers). At a young age, collagen fibers are quite strong and provide the skin with mobility and flexibility, while maintaining its elasticity and shape. All this can be compared to an armored bed, the base of which is a metal mesh. While the bed is new, the iron springs quickly return to their original position, but over time the springs begin to sag and the bed loses its shape. It’s the same with our skin - while we are young, our springs (collagen fibers) keep their shape perfectly, but with age they begin to sag. The matrix (matrix or amorphous component) in its structure most closely resembles a gel and consists of polysaccharides. The most famous of them are chitosan, seaweed polysaccharides, and hyaluronic acid. It is the components of the extracellular matrix, both amorphous and fibrillar, that create the skin from the inside. The saccharides themselves do not form fibers, but they fill all the spaces between the connective cells and fibers. It is through them that the interstitial transport of all substances occurs. As a result, it is the condition of the dermis (water content in the polysaccharide gel, the integrity of collagen fibers, etc.) that determines the condition of the epidermis and the healthy appearance of the skin.
Drawing of massage lines
And the last thing we will touch on is the hypodermis or subcutaneous fatty tissue - the deepest layer of the skin. It consists of loose connective tissue, which contains many fat cells. The thickness of this layer varies and depends on lifestyle, nutrition, and metabolism. Fat is involved in thermoregulation and thermal insulation processes, preventing the body from overcooling or overheating, and also protects tissues and organs from mechanical influences. Fat cells are also depots in which fat-soluble vitamins (A, E, F, K) can be stored. Subcutaneous fatty tissue is very important as a mechanical support for the outer layers of the skin. Skin in which this layer is poorly expressed usually has more wrinkles and folds and ages faster.
Why is it so important to learn and always apply the Langer line rule?
Nothing preserves beauty and youth better than careful skin care and care from birth! Of course, every age has its own rules. The most important thing is not to miss the moment and prevent the premature appearance of wrinkles!
It would seem that everyone has heard about the existence of some mythical massage lines through which any cosmetic procedures must be performed. But, nevertheless, even those who know and have heard do not always follow this rule.
And in vain.
Of course, if you apply the same cream 1-2 times not along the massage lines, no disaster will happen. But the fact is that you apply the cream at least 2 times a day, which means 365*2=730 times during the year!
Therefore, you need to learn these lines, then integrate this skill into your life so that it becomes your useful habit!
To understand the very essence of this concept - the Langer line, I present to your attention a small encyclopedic reference:
“The lines of least stretch of the skin were discovered as a result of a study of the elastic properties of the skin by the German anatomist Langer in 1861. Therefore, experts call these lines Langer's lines.
The essence of this discovery is that collagen fibers in the skin do not lie randomly, but in a certain order. The stretchability of the skin depends on this - along the Langer lines the skin stretches 3 times less than across it. Wounds will form a smaller scar if the wound occurs along this line. Plastic surgeons and cosmetologists use this fact in their work.”
✅all movements of your hands on your face - whether you are applying cream, a mask, removing makeup or washing your face - should be done along massage lines☝
✅treat your skin as carefully as possible, because rough touches stretch the skin and make it sluggish
Science has known for quite some time about the existence of such a substance as collagen. These are protein threads present in connective tissue, namely in the intercellular substance. Collagen provides firmness and elasticity to fibers. This substance forms peculiar bundles. Langer lines are located in their direction.
History of discovery and subsequent research
In 1861, the scientist Langer published his work “On the anatomy and physiology of the skin. On the splitting of the skin." It was in it that he described the presence of conditionally drawn lines on the surface of the skin, along which it is most extensible.
Langer studied the properties of skin, such as elasticity, and noticed that skin is more stretchable in some directions than in others. He associated this phenomenon with the placement of collagen bundles under the skin in these places. He stated that in different places of the body, elastic fibers have different directions.
Along the Langer lines (cleavage lines) the strength of the skin is much higher. The scientist established this experimentally, using skin on corpses. In our time, researchers have tried to provide more accurate data about this phenomenon by doing experiments on animal skin. Of course, animal skin is significantly different from human skin. Therefore, the information obtained in this way left many questions.
Scientists at University College Dublin in Ireland and Professor Aisling Ni Annaidh personally tried to obtain accurate information. To conduct research, they needed about fifty-six skin fragments (taken from cadaveric material).
These studies confirmed Langer's hypotheses, but the question of the origin of this phenomenon remained open. This is probably simply a matter of the forces that act when attaching the skin to the body, but it could also be an anatomical phenomenon. That is, it is possible that the skin itself has hidden structures that form Langer's lines.
The main conclusion from all the studies of this phenomenon can be the fact that the existence of Langer lines simply needs to be taken into account by many specialists in different fields. From surgery to cosmetology, for a more effective effect on the skin you need to know the specifics of Langer's lines.
Langer lines on the face
To reduce the consequences after surgery, including plastic ones, as well as for more effective work of a cosmetologist, it is necessary to know where exactly the Langer lines are located on the face.
These lines on the face are located as follows:
- Along the line from the chin to the earlobes.
- From the corners of the lips to the middle of the ears.
- From the wings of the nose to the upper tips of the ears.
- From the middle of the nose to the temples.
- On the nose: from the tip of the nose to the bridge of the nose along the back and from the back of the nose to the wings.
- Upper eyelid: in a semicircle from the inner corner of the eyelid to the outer.
- Lower eyelid: in a semicircle from the outer corner of the eyelid to the inner.
- Forehead: from the middle of the forehead to the temples; from the eyebrow line vertically upward to the hairline.
- Neck: The front surface of the neck has an arrangement of fibers from bottom to top, while the side surface has fibers from top to bottom.
It is not so difficult to remember the location of these lines, but they should definitely be taken into account when cleansing your face and removing makeup, and even when applying make-up. These procedures should be carried out strictly in the direction of these lines, avoiding stretching the skin. Applying makeup to the surface of the nose is from the wings vertically to the base of the nose, and starting from the forehead, change the direction towards the temples.
The skin around the eyes is the thinnest and should never be stretched when applying or removing makeup. It is better to rub in the products with patting movements, and remove makeup with circular massage movements. Applying cosmetics to the face should occur along stretch lines, which will keep the skin more elastic. Proper care prevents the appearance of wrinkles.
Langer lines on the body and head
It is obvious that collagen bundles are located in a certain direction not only on the face, but throughout the body. For a better understanding, you should consider the drawing.
Langer's lines on the body are usually located in places where the skin naturally folds, since they are directed perpendicular to the muscles so that when the muscles are tense, the collagen bundles are not damaged. As we can see, Langer's lines are located horizontally on the hands, parallel to each other. Also in the center of the back and on the back of the legs. The lines run parallel to the ribs, bend around the pectoral muscles in front and the shoulder blades in the back. On the buttocks, directed from the center to the edges from bottom to top. On the front of the leg above the knee, the lines are located vertically. All these features are usually taken into account by surgeons during operations, massage therapists and cosmetologists.
When we need to determine the location of Langer's lines in places where there are no natural folds or wrinkles, we can do the following: squeeze an area of skin with your fingers, first along and then across. If skin folds appear, then Langer's lines are located there; if the surface is smooth, this area does not correspond to the direction of the lines.
Langer's lines are located not only on the face, but throughout the head. Their location is important to consider when undergoing hair transplantation, for example.
Langer's lines in the upper half of the forehead are parallel to the hairline.
The facial massage procedure is useful because it activates blood circulation and lymphatic drainage in the skin, which leads to an improvement in its condition. Also, when acting through the skin on the muscles through massage movements, you can remove the clamps in them, tone them, returning the natural youthful oval of the face. For a professional high-quality massage, a specialist must have certain qualifications and know where the facial massage lines are located.
In order not to stretch, but to tighten the skin, to give it elasticity during massage, applying cream and removing makeup, you need to know what the location of massage lines is on the face and neck.
Massage lines were discovered by the German scientist Karl Langer, who studied the structure of human skin and its elastic properties. “Langer lines” go in the direction of more elastic stretching of the skin.
Scheme of massage lines for the face and neck:
Location of massage lines:
- Line for neck massage, from the bottom of the neck along to the chin;
- From the middle of the chin to the earlobes in a smooth semicircular line, in both directions;
- From the middle of the top of the lip to the top of the ear in a smooth semicircular line;
- The nose is massaged from tip to bridge;
- Massage around the wings of the nose from the lip to the top of the wings;
- The cheeks are massaged from the nose to the upper tips of the ears;
- The lower eyelid is massaged from the outer corner of the eye to the inner, the upper eyelid is massaged from the inner corner to the outer;
- The forehead is massaged from the bridge of the nose with fan movements to the hairline.
Before the massage, a necessary condition is to clean the skin of makeup. The massage is performed with rich natural cream or oil.
Surgical incisions on the face.
Topography of the temporal region. Scheme of cranial topography. Projection of the middle meningeal artery. Osteoplastic and decompressive craniotomy. The temporal region is delimited from the orbit by the zygomatic process of the frontal and the frontal process of the zygomatic bones, and from the lateral region of the face by the zygomatic arch. The upper border is determined by the contour of the upper edge of the temporal muscle. The skin is thinner than in the fronto-parietal-occipital region; the hairline remains in the posterior part of the region, less firmly fused with the superficial fascia, especially in the anterioinferior part. Blood supply: The frontal branch of the superficial temporal artery anastomoses with the supraorbital artery. The parietal branch of the superficial temporal artery anastomoses with the occipital artery. In addition, the branches of the left and right superficial temporal arteries anastomose with each other. Innervation: Sensitive innervation - n. auriculotemporais, n. zygomaticotemporalis, r. frontalis, r. zygomaticus - branch of the facial nerve. In the tissue between the plates of the superficial fascia pass the trunks of the superficial temporal vessels and branches of the auriculotemporal nerve, n. auriculotemporalis, as well as the motor branches of the facial nerve, rr. frontalis et zygomaticus. The fascia of the temporal region has the appearance of an aponeurosis. Attaching to the bones at the borders of the region, the fascia closes the temporal fossa on the outside. Between the superficial and deep layers of the temporal fascia there is interaponeurotic fatty tissue. Under the temporal aponeurosis there is the temporal muscle, vessels, nerves and fatty tissue, in the space between the anterior edge of the temporal muscle and the outer wall of the orbit there is the temporal process of the fatty body of the cheek. Anterior and posterior temporal vessels and nerves, a., v. et n. temporales profundi anteriores et posteriores. The deep temporal arteries arise from the maxillary artery, and the nerves arise from n. mandibularis. Lymph flows into the nodes in the thickness of the parotid salivary gland - nodi lymphatici parotideae profundi. On the inner surface of thinned bones (temporal squama and large wing of the sphenoid bones) a. meningea media. Under the dura mater are the frontal, parietal and temporal lobes of the brain, separated by the central (Rolandic) and lateral (Sylvian) fissures. Scheme of cranial topography. The diagram makes it possible to project onto the surface of the cranial vault the main grooves and convolutions of the cerebral hemispheres, as well as the course of the trunk and branches of a. meningea media. A midsagittal line of the head is drawn connecting the glabella, glabella, with the protuberantia occipitalis externa. The main-lower horizontal line is drawn, running through the lower orbital edge and the upper edge of the external auditory canal. An upper horizontal line is drawn parallel to the lower one - through the supraorbital edge. Three perpendiculars are restored to the horizontal lines: the anterior one - to the middle of the zygomatic arch, the middle one - to the middle of the articular process of the lower part and the posterior one - to the posterior border of the base of the mastoid process. The projection of the central (Rolandic) sulcus is a line drawn from the point of intersection of the posterior vertical of the midsagittal line to the intersection of the anterior vertical of the upper horizontal line. The lateral (Sylvian) fissure, sulcus lateralis, is projected onto the bisector of the angle formed by the projection of the central (Rolandian) fissure, sulcus centralis, and the upper horizontal thalia. Barrel a. meningea media is projected at the point of intersection of the anterior vertical with the lower horizontal (at the upper edge of the zygomatic arch, 2.0-2.5 cm posterior to the frontal process of the zygomatic bone). Frontal branch a. meningea media - to the point of intersection of the anterior vertical with the upper horizon, and the parietal branch - to the place of intersection of this horizontal with the posterior vertical. Decompressive trephination. Produced when intracranial pressure increases in cases of inoperable brain tumors, with progressive cerebral edema developing as a result of injury. The patient is on the left side, the leg on this side is slightly bent at the knee and hip joints. A horseshoe-shaped incision of the skin and subcutaneous tissue in the right temporal region, corresponding to the line of attachment of the temporal muscle. The flap is separated and turned to the base at the level of the zygomatic arch. The temporal aponeurosis, interaponeurotic fat cell and temporal muscle are dissected in the vertical direction to the periosteum. The latter is dissected and separated with a rasp on an area of 6 cm2. Having opened the wound with hooks, a milling hole is made in the center of the area freed from the periosteum with a large cutter and then it is expanded with forceps-nippers. The expansion of this hole in the antero-inferior direction is dangerous due to the possibility of damage to the trunk a. meningea media. Before opening the dura mater, a lumbar puncture is performed. Cerebrospinal fluid is removed in small portions (10-30 ml) to prevent wedging of the brainstem into the foramen magnum. The dura mater is opened with a cruciform incision and additional radial incisions. The surgical incision is sutured layer by layer, with the exception of the dura mater; it remains unsutured. Osteoplastic craniotomy. Indications: for the purpose of access for surgery on its contents during strokes, to stop bleeding from damaged a. meningea media, removal of intracranial hematoma and inflammatory focus or brain tumor. A Krenlein diagram is applied to the operated area. A horseshoe-shaped incision with the base of the flap at the zygomatic arch is made so that the trunk and posterior branch of a can be ligated in the burr hole. meningea media. According to the lines outlined in Krenlein's diagram, the skin, subcutaneous tissue and temporal aponeurosis are dissected, and in the lower parts of the anterior and posterior parts of the incision, the temporal muscle is divided along its bundles. The length of the base of the flap is at least 6-7 cm, its edges are 1 cm from the edge of the orbit and the tragus of the ear. After stopping the bleeding, the musculocutaneous aponeurotic flap is turned down onto gauze napkins and covered on top with gauze moistened with a 3% hydrogen peroxide solution. The cutting out of the osteoperiosteal flap begins with an arcuate dissection of the periosteum, departing 1 cm from the edges of the skin incision. The periosteum is peeled off from the incision in both directions to a width equal to the diameter of the cutter, which is then used to make 5-7 holes. The areas between the cutter holes are cut with a Gigli saw or Dahlgren pliers. Topography of the deep facial region. Fascia and cellular spaces. Ways of spread of purulent streaks on the face. Interventions for purulent processes on the face. Borders: above - the large wing of the sphenoid bone, in front - facies infratemporalis tuber maxillae. The parotid salivary gland is adjacent to the back, and below it closes at the place of attachment to the angle of the lower jaw of the masseter and medial pterygoid, m. pterygoideus medialis, muscles. Cellular spaces: spatium tempororterygoideum between the temporal and lateral pterygoid muscles, contains the maxillary artery, a. maxillans, and venous pterygoid plexus; spatium interpterygoideum - between the lateral and medial pterygoid muscles, contains n. mandibular!* and its branches: nn. auriculotemporal, buccalis, lmgualis et alveolaris inferior; a. buccalis, The interpterygoid fascia covers the outer surface of the medial pterygoid muscle. It is pierced by the inferior alveolar neurovascular bundle, a., v. et n alveolares mfcnores. The venous pterygoid plexus anastomoses with the cavernous sinus of the dura mater through the emissary vein of the anterior lacerated foramen, as well as through an anastomosis that penetrates through the inferior orbital fissure and flows into the inferior ophthalmic vein. These venous connections are of great importance in the development of intracranial complications during inflammatory processes in the facial area. From the pterygoid plexus, blood flows into the mandibular vein, v. retro-mandibularis, which, upon exiting the parotid salivary gland, merges with the facial gland, which flows into v. jugulans interna. Interventions for purulent processes on the face. Most acute inflammatory processes on the face are treated conservatively. When conservative treatment is ineffective, puncture of the infiltrate with antibiotic solutions and incisions are used. The purpose of the operation is to create an outflow of pus when the lesion has formed in order to prevent the spread of the inflammatory process. Before opening the purulent focus, a diagnostic puncture is performed in the center of fluctuation. An incision is made above the center of fluctuation in the area of the purulent focus. Perimaxillary phlegmons, which develop in connection with dental caries, are often opened using intraoral approaches. Abscesses of the nasolabial fold and parotid area are opened with external incisions. In this case, only the skin with subcutaneous tissue is dissected. They pass through the deep layers of subcutaneous tissue and facial muscles, bluntly pushing apart the tissue with closed scissors and anatomical tweezers. Topography of the fronto-parieto-occipital region. Features of blood supply to the integument of the cranial vault. Technique of primary surgical treatment of non-penetrating and penetrating wounds of the cranial vault. In the cranial vault, the following areas are distinguished: unpaired - frontal, parietal, occipital and paired - temporal and mastoid areas. Due to the similarity of the anatomical structure, the first three regions are combined into one - fronto-parieto-occipital, regio frontoparietooccipitalis. Borders: anteriorly along the supraorbital margin, margo supraorbitalis, posteriorly along the superior nuchal line, line anuchae superior, in the lateral sections along the superior temporal line, linea temporalis superior. The skin of most of the area is covered with hair. It is inactive due to its strong connection by numerous fibrous cords with the underlying tendon helmet (supracranial aponeurosis), galea aponeurotica (aponeurosis epicranius). Subcutaneous tissue is represented by cells between the indicated connective tissue strands, densely filled with adipose tissue. The tendon cap is weakly connected to the periosteum and is separated from it by a layer of loose fiber. This explains the often scalped nature of wounds of the cranial vault. In this case, the skin, subcutaneous tissue and tendon helmet are completely peeled off over a greater or lesser extent from the bones of the cranial vault. Neurovascular formations are located in the subcutaneous tissue, and the adventitia of the blood vessels is firmly fused with connective tissue bridges that divide the tissue into cells. Even small wounds of the skin and subcutaneous tissue are accompanied by severe bleeding from these gaping vessels. When providing first aid, bleeding is stopped by pressing the wounded vessels to the bones of the skull. Blood supply and innervation: supraorbital vessels and nerves, a., v. et n. supraorbitales, occipital artery, a. occipitalis, greater occipital nerve, n. occipitalis major, lesser occipital nerve, n. occipitalis minor (sensitive branch from the cervical plexus), a., v. et n. supratrochleares. The veins of the soft tissues of the fornix, intraosseous and intracranial veins form a single system, the direction of flow in the blood of which changes due to changes in intracranial pressure. The veins here have no valves. Lymph flows to three groups of lymph nodes: from the frontal region - into the superficial and deep parotid lymph nodes, nodi lymphatici parotidei superficiales et profundi; from the parietal region - to the mastoid, nodi lymphatici mastoidei; from the parietal and occipital regions - to the occipital lymph nodes, nodi lymphatici occipitales. Hematomas and inflammatory infiltrates, widely distributed in the subgaleal space (within the boundaries of the tendon cap), in the subperiosteal tissue remain limited to one skull bone. Technique of primary surgical treatment of wounds of the cranial vault Wounds of the cranial vault can be non-penetrating (without damage to the dura mater) and penetrating (with damage to the dura mater). In case of blunt trauma, the inner plate of the skull bones undergoes the most severe changes, then a fracture of the outer plate occurs. A fracture of the skull bones can be in the form of a crack, fissure, comminuted, depressed fracture. For linear fractures in the form of a crack, surgery is indicated when fragments of the internal plate are displaced. For comminuted and depressed fractures, indications for surgery are available regardless of the presence of symptoms of damage to the dura mater and brain. The purpose of the operation is to stop bleeding, remove foreign bodies, prevent the development of infection in soft tissues, bones and in the cranial cavity, and also prevent damage to the brain that prolapses into the wound during traumatic swelling. During the initial treatment of a skull wound, after preparing the surgical field, the wound is mechanically cleaned, all non-viable tissue is removed, bleeding is stopped, and blood clots are removed; the edges of the bone defect are given a smoothed appearance; remove brain debris, blood clots and foreign bodies from a brain wound. Excision of the edges of the wound is carried out sparingly - to the bone to a width of 0.3 cm, stopping the bleeding first by pressing with fingers, and then applying clamps to the bleeding vessels, followed by ligation or coagulation. In case of comminuted fractures, loose bone fragments and foreign bodies are removed. Luer cutters are used to bite off the edges of the bone defect until an intact dura mater appears. Remove fragments of the inner plate that may be under the edges of the burr hole. Treatment of wounds of the dura mater. If the dura mater is not damaged and pulsates well, it should not be dissected. If a subdural hematoma is visible through the tense, weakly pulsating dura mater, it is aspirated through a needle. If blood clots are not removed in this way, the dura mater is cut crosswise. Removal of destroyed brain tissue, superficially located bone fragments and subdural hematoma is carried out by carefully rinsing with a stream of warm isotonic sodium chloride solution. The wound of the dura mater is sutured with thin silk ligatures, the bone flap during osteoplastic trephination is connected to the bone with catgut sutures passed through the tendon helmet and periosteum, thin silk or threads made of polymer material, the edges of the skin wound are connected with silk interrupted sutures. Drainage is inserted into the subgaleal tissue under the edges of the skin-aponeurotic incision before suturing. Topography of the mastoid region. Trepanation of the mastoid process. The mastoid area is located behind the auricle and is covered by it. The boundaries correspond to the outlines of the mastoid process, which can be easily palpated. From above, the border is formed by a line that is a posterior continuation of the zygomatic process of the temporal bone. To project the intraosseous formations of the process, its outer surface is divided into 4 quadrants by two lines: a vertical line is drawn along the height of the process from the apex to the middle of its base; a horizontal line divides this vertical in half. The cave, antrum mastoideum, is projected onto the anterosuperior quadrant, the bony canal of the facial nerve, canalis facialis, onto the anterosuperior quadrant, the posterior cranial fossa into the posterosuperior quadrant, and the sigmoid venous sinus is projected onto the posteroinferior quadrant. The subcutaneous tissue often contains bundles of the posterior auricular muscle, the posterior auricular artery and vein, a. et v. auriculares posteriores, posterior branch of the great auricular nerve, n. auricularis magnus (sensitive branch from the cervical plexus), posterior auricular branch of the facial nerve, r. auricularis posterior n. facialis. Under the aponeurosis formed by the tendon of the sternocleidomastoid muscle, nodi lymphatici mastoideae, which collect lymph from the parieto-occipital region, from the back surface of the auricle, from the external auditory canal and the eardrum. The occipital artery, a. occipitalis. The periosteum is firmly fused with the outer surface of the mastoid process, trepanation triangle (Shipo), where the periosteum easily peels off. The boundaries of the Shipo triangle are in front the posterior edge of the external auditory canal and spina suprameatica, in the back - crista mastoidea, and above - a horizontal line drawn posteriorly from the zygomatic process of the temporal bone. Within the triangle of Shipo there is a resonating cavity - the mastoid cave, which communicates through the aditus ad antrum with the tympanic cavity. Trepanation of the mastoid process, mastoidotomia, antrotomia Indications: purulent inflammation of the middle ear, complicated by purulent inflammation of the cells of the mastoid process. The purpose of the operation is to remove purulent exudate, granulations from the air cells of the mastoid process, to open and drain the mastoid cave, antrum mastoideum. Anesthesia - anesthesia or local infiltration anesthesia with a 0.5% novocaine solution. Position of the patient on his back; the head is turned to the healthy side; the auricle is pulled anteriorly. The skin with subcutaneous tissue is dissected parallel to the attachment of the auricle, moving 1 cm posteriorly from it. The projection of the Shipo trepanation triangle is first determined. The projection of the triangle should be in the middle of the operational approach. By stretching the edges of the skin incision with a retractor, a trepanation triangle is exposed on the anterior surface of the upper inner quadrant of the mastoid process. The trepanation of the special process within this triangle begins with the separation of the periosteum by a departure by a departure. A sufficient opening of the cave is controlled by a button zone, which is examined by the walls of the cave, and carefully leave it through Aditus Ad Antrum into the drum cavity. The pus contained in the cave and other cells and granulations are removed with an acute spoon. The wound is sutured above and below the graduate left in the cave (a strip of glove rubber). Topography of the whimsical and yielding region. Distribution of purulent bastards with mumps. Operations in acute purulent mumps. The skin is thin, in men it is covered with hair. The subcutaneous tissue of the penetration is with connective tissue leggings connecting the skin with their own fascia-Fascia Parotideomasseterica. The fascia of the region forms a case of the chewing muscle, which is converted to the fascial capsule of the fatty body of the cheek. On the outer surface of the chewing muscles in the transverse direction, there are DUCTUS PAROTIDEUS, a. et v. Transversa Faciei and buccal branches of the facial nerve. Between the chewing muscle and the branch of the lower jaw there is a chewing and chelulous space made by loose fiber. The chewing and chelulous space continues under the zygomatic arc up on the outer surface of the temporal muscle to the place of fixing it to the inner surface of the temporal aponeurosis. Own fascia of the side regional faces, splitting, forms the capsule of the parotid salivary gland. Pluting salivary gland, GL. Parotis, fills the halter. The surface part of the parotid salivary gland in the form of a triangle facing the base to the zygomatic arc is located on the outer side of the chewing muscle. The output duct of the parotor gland goes in the transverse direction at a distance of 1.5- 2.0 cm below the zygomatic arc. The fascial capsule is poorly developed on the upper surface of the gland adjacent to the outer auditory passage, and on the inside of the Pars Profunda of the parotid gland, facing the anterior winding space. With purulent inflammation of the parotid salivary gland (mumps), the pus breaks 4 times more often into this space, to the wall of the pharynx than into the outer auditory passage. In the thickness of the parotid salivary gland, two nerves pass - n. Facialis and N. auriculotemporalis, outer sleepy artery, its final branches and v. Retromandibularis; The parotid lymph nodes are deep in the thickness of the glands and superficial ones to fascia. RR depart from the upper branch of the facial nerve. Temporalis, zygomaticus et buccallis; from the lower r. Marginalis Mandibulae and R. Colli. In the thickness of the gland, the connections between the branches of the facial nerve are formed by Plexus parotideus. Operation in acute purulent mumps. Anesthesia - anesthesia. The purpose of the operation is to open a purulent-non-chorotic focus, drainage of the wound to complete rejection of necrotic tissues. After processing the operating field, the skin, subcutaneous fiber and Fascia Parotideomasseterica are dissected over the place of the proposed cluster of pus. The incision is carried out parallel to the facial branches of the facial nerve. The tissue of the gland above the abscess is pushed in a blunt path. Drainage is brought to the purulent-nonsense focus. Topography of the surface formations of the lateral region of the face. Features of the venous outflow of the region are venous anastomoses, their value in the spread of purulent infection. The direction of the spread of inflammation during phlegmon of the face to the caveat venose sinus in cases where venous anastomoses are not involved in the process. The fatty body, adjacent to the upper and lower jaws, serves as a conductor of inflammatory processes, primaryly developing in the jaws (odontogenic origin). Build muscle, m. Buccinator. The outer surface of the buccal muscle is covered with a dense bush-flavor fascia, the internal with a mucous membrane. On the outer surface of the buccal muscles pass n. Buccalis (from n. Mandibularis), buccal vessels and small facial lymph nodes are located (Nodi Lymphatici Buccinatorius).
surgical incisions on the face.
Borders: above - the zygomatic arch and the lower edge of the orbit, below - the lower edge of the lower jaw, in front - the nasobuccal and nasolabial folds, the angle of the oral fissure, behind - the edge of the ramus of the lower jaw. The superficial lateral region of the face is divided into the buccal, regio buccalis, and parotid-masticatory, regio parotideomasseterica regions. Inward from the branch of the lower jaw is the deep region of the face, regio facialis profunda. External landmarks. The zygomatic bones are located below the lateral corners of the eyes. Posteriorly, the zygomatic bone passes into the zygomatic arch, arcus zygomaticus. The suborbital margin is palpated medially from the zygomatic bone. Anterior to the tragus, the articular process of the mandible and the temporomandibular joint are palpated. The masticatory muscle is contoured on the outer surface of the lower jaw branch. Along the midline of the body of the lower jaw there is an individually developed mental protrusion, protuberantia mentalis, on the sides of it there are mental tubercles, tuberculi mentales. The facial arteries and vein are projected from the intersection of the anterior edge of the masticatory muscle with the lower edge of the lower jaw in an ascending direction to the inner corner of the eye. Along this line, approximately at the level of the wing of the nose, the most important anastomosis of the facial vein with the pterygoid venous plexus is determined.
Direction of surgical incisions on the face. When performing operations on the face, the direction of the skin incisions must coincide with the location of the natural folds of the skin. A scar is least noticeable if it imitates a new wrinkle or is located in an existing fold of skin. The appearance of a postoperative scar largely depends on the exact approximation of the dissected muscles, subcutaneous tissue and skin, as well as on the location of the scar in the physiological folds and wrinkles on the face. Surgical treatment of facial wounds consists of applying a primary blind suture, regardless of the period of initial treatment of the wound. It is necessary to accurately compare the edges of the wound, avoiding facial asymmetry. The entire thickness of the subcutaneous tissue is carefully sutured using submerged catgut sutures. Sutures placed on the subcutaneous tissue bring the skin edges of the wound into contact and prevent the folding of these edges.
How to do a facial massage
Before starting the massage, the skin on your face should be thoroughly cleaned and your hands should be washed thoroughly. The product you must choose is natural, without chemical ingredients.
When performing self-massage of the face, you should adhere to the rule of the four “Ps”:
- Punching;
- Pat;
- Tingling;
- Stroking.
All these movements should be carried out along the lines for facial massage with cream or oil applied to the skin.
- You need to start self-massage by pressing the skin with your fingertips;
- Then you should proceed to gentle rubbing in a circular motion in the direction of the massage lines;
- Next comes intense kneading of the skin and muscles underneath;
- Then pats;
- Finish the session with vibration and stroking.
Acupressure facial massage
During the procedure, acupressure may also be used. It consists of point pressure on strictly defined muscle areas. Such points are called active. Their stimulation helps to activate blood circulation, eliminate swelling, improve skin tone, which leads to the launch of a rejuvenation mechanism.
Here are some points whose regular massage will help in facial rejuvenation:
- in the center of the forehead (responsible for eliminating wrinkles in this area);
- on the inner and outer corners of the eyes;
- between the eyebrows in the bridge of the nose (light pressure on it can not only smooth out wrinkles on the forehead, but also generally improve well-being);
- in the center of the eyebrows, as well as along the entire eyebrow;
- on the temples (for headaches and lack of concentration);
- under the cheekbone lines;
- near the corners of the lips;
- under the nose and points near the wings of the nose;
- under the chin;
- under the lower lip (stimulation promotes relaxation and calmness).
Ideally, massage sessions should be performed daily. If this is not possible, then the option of a procedure every two to three days will also be good for improving the condition of the face.
Also on our website “Eco-Youth” you can read about the existence of...