Demodicosis is a serious skin disease that affects 3.5% of the inhabitants of our planet. Demodicosis is very similar in appearance to acne. Many people do not pay enough attention to treating the disease, believing that it will go away on its own. But demodicosis as a disease is dangerous due to its complications, and therefore requires comprehensive and thorough treatment.
Demodicosis resembles acne
General information about demodicosis
Demodicosis is acarodermatitis. This term means that the disease is caused by ticks. The main causative agent of the disease is the acne gland or demodex. Parasites can live in humans and other mammals. The size of the mites ranges from 0.2 to 0.5 mm; they settle in the ducts of the sebaceous glands and near the hair follicles. Parasites are located on the skin of the face (eyelids, brow ridges, forehead, nasolabial folds, chin), in the external auditory canal, in the upper back, on the chest. Any person can become a carrier of a tick, but not all carriers develop demodicosis.
At the initial stage of the disease, formations similar to acne appear on the skin. The parasitic infection gradually develops, the affected areas increase in size. Squashing acne makes the situation worse because microorganisms begin to get into the open wounds, and the mites are pressed into the deeper layers of the skin.
It is very difficult to treat demodicosis; there are tablets for demodicosis, special ointments and hardware therapy methods.
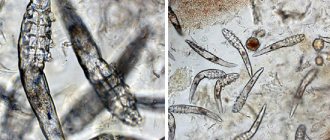
Demodicosis is caused by the demodex mite.
How to cure demodicosis several times faster?
* The results of using the products are individual and may vary depending on the degree of skin damage, the number of relapses suffered, the state of local immunity, etc.
| How long does it take to treat demodicosis of the face? On the Internet I found a method that promises to get rid of demodicosis in 1-2 weeks. |
| Answered by cosmetologist Ekaterina Belykh If you are offered to defeat demodicosis in one or two weeks with the help of some “miracle remedy,” then you are dealing with charlatans and here’s why: |
Demodicosis is a serious disease.
An important requirement for successfully combating the disease is to comply with the timing of treatment for demodicosis. Only in this case is the complete destruction of parasites guaranteed and the prevention of relapses.
When treating facial skin for demodicosis, the most frequently asked question is: “Is a quick recovery possible?” How long does it take to treat demodicosis in people?
A new method of treating demodicosis with specialized products “Demodex Complex®” is the fastest and safest way to treat demodicosis. The full course of treatment lasts from 3 to 5 months (depending on the type of subcutaneous mite that affects the skin). These dates are not accidental; they are determined by the natural processes of the parasite’s life: one life cycle of demodex is 25 days; to destroy the mite colony, it is necessary to continue continuous treatment of demodicosis throughout the life of all three generations. Thus, the so-called “long” demodex is destroyed in 3 months. If “short” demodex is detected on the skin, the treatment period will need to be increased. This is due to the fact that this type of subcutaneous mite lives deeper in the sebaceous glands. The treatment period for “short” demodicosis will be 5 months.
It is important to understand that the presence or absence of a “short” mite can only be confirmed by a laboratory test for demodicosis. If you have not been tested, then when treating you need to focus on a period of 5 months.
Any reduction in the course affects the effectiveness of treatment and inevitably leads to relapse.
If the prescribed treatment time is not followed, the disease can drag on for several years and become chronic. In order to prevent the disease from becoming intractable, it is necessary to strictly adhere to all instructions. It is important to take into account that healing is achieved only with continuous use of drugs according to the developed regimen.
Continuity is a must for successful treatment! Make sure that you always have the required amount of cosmetics against demodicosis in stock. Interrupting treatment even for 1 day will require starting treatment from the very beginning.
So, how long does it take to treat demodicosis of the face? A final cure is only possible if the demodex mite colony is completely destroyed. The full course will take from 3 to 5 months. How quickly you cure demodicosis on your face depends on many different factors: the duration of the disease, previously used medications, skin type, how weakened your immune system is, whether you use decorative cosmetics, etc. However, there are some patterns that can be noticed during therapy : improvement in condition and elimination of symptoms begins almost immediately.
Already in the 1st week, patients will see noticeable results: after using the Xinsheng cream, the itching will instantly stop, and the next morning all pimples that have not been treated in any way will begin to dry out and decrease. With the application of Kang cream, pleasant sensations will appear, and the skin will become noticeably smoother. Such a quick effect will certainly please you and make you want to complete the full course of treatment. Each patient, having noticed the first results, will be able to note that demodicosis is curable and it is possible to cure it quickly.
At 2-3 weeks, the most difficult period of treatment will begin: new rashes will appear, skin oiliness will increase and, in general, this may seem like a “deterioration” of the general condition. This stage is very short, on average only 2–3 days. Some patients may panic and stop treatment, but this is precisely their main mistake! All these symptoms are not a deterioration at all, but, on the contrary, the most important stage of treatment. The creams kill the mites on the face, the treatment works, and they begin to decompose under the skin, thereby causing inflammation. Through newly formed pimples, the decay products of mites are removed and the skin is cleansed. This process means that creams from the Demodex Complex® series have begun to effectively treat facial demodicosis. As you pass this stage, the skin will begin to exfoliate and the first tender and healthy areas will begin to appear, and soon the entire skin will become smooth and radiant with health!
At the 4th week of treatment, the skin will begin to look more beautiful and well-groomed. At this stage, patients will see real treatment results, which can only be achieved using Demodex Complex® drugs. At this stage, you can already share reviews about “how I got rid of demodicosis on my face.” But in no case should the course of treatment be completed after the end of the 1st month, no matter how serious the visible results may be.
Over the course of 5-7 weeks, small rashes will still appear, but there will be much fewer of them, because most of the mites will be destroyed the first time. At the same time, the face after demodicosis will look much healthier, smoother, and redness will disappear. A healthy complexion and well-groomed skin will not go unnoticed; patients will receive pleasant compliments from others.
At the 8th week, in most patients, the skin will look completely healthy and only the client’s picky eye will be able to find minor flaws on it, and even these will soon be completely gone. At this stage, it is very important not to stop treating demodicosis, but to bring it to the very end, that is, to be treated for 3 to 5 months. Then all subcutaneous mites will be destroyed forever! Specialized Demodex Complex® products not only help with such a complex question of “how to get rid of demodicosis”, but also reliably protect against its recurrence.
After completing the full course of treatment, demodicosis goes away and patients will be able to live a full life again, enjoying their health and beauty!
Factors stimulating the development of the disease
Demodicosis usually appears in adolescence and often affects pregnant women. This indicates that the disease does not develop on its own. Infection occurs against the background of disturbances in the body. Activation of demodexes in the skin is provoked by various internal and external factors. Internal ones include:
- hormonal imbalances (increased or decreased secretion of sex hormones, adrenaline, thyroid hormones),
- weakened immunity (the immune system is unable to respond to a parasitic infection),
- diseases of the gastrointestinal tract.
External factors stimulating mite activity:
- hormonal ointments (their use reduces local skin immunity),
- excessive exposure to ultraviolet radiation,
- the effect of hot water and steam (bath procedures).
Swimming in too hot water activates parasitic mites
Demodectic mange on the face: symptoms
The mites that cause the disease are often found on the skin of healthy people and are classified as human saprophytes. Pathology develops with an increase in the number of parasites. Active reproduction is caused by exogenous and endogenous factors, somatic diseases that occur with impaired immunity.
The danger of Demodex mites is that they are carriers of microbes and viruses that cause pathological processes on the skin of the face. Symptoms of the disease are divided into objective and subjective.
The latter include the patient’s sensations and complaints:
- itching sensation, especially in the eyebrows and forehead;
- burning sensation, “creepy crawling”;
- feeling of a foreign body, pain in the eyes;
- accumulation of pus in the eyelid area in the morning;
- loss of eyelashes, redness of the eyelids;
- increased greasiness, redness of the dermis.
Objective symptoms are identified by a doctor; they depend on the severity of the disease, skin type, and body condition:
- inflammatory reaction and infiltration of the skin of the face and around the eyelashes;
- dry dermis, large-plate peeling;
- papule and papulovisicles of conical shape;
- severe inflammation caused by dilation of capillaries;
- infiltration of the conjunctiva, purulent crusts around the eyelids.
Treatment methods are determined based on the clinical picture and diagnostic results.
Symptoms of demodicosis
Demodectic mange is easily confused with acne and some other types of dermatitis. They are similar in symptoms. General manifestations of demodicosis:
- Skin inflammation.
- Red spots.
- Formation of nodules, bumps, and rosacea on the skin.
- Enlarged pores.
- Peeling.
Distinctive features of demodicosis:
- seasonal exacerbations (spring and autumn),
- itching, which worsens in the evenings and after exposure to heat.
Demodicosis often develops in the sebaceous glands on the skin of the eyelids. Symptoms of eyelid damage by Demodex cannot be confused with another disease. These include:
- Inflammation of the eyelids.
- The appearance of purulent nodules and crusts along the edges of the eyelids.
- Feeling dry.
- Eyelash loss.
- Clumping of eyelashes.
A prolonged inflammatory process on the eyelids can lead to the development of conjunctivitis.
If any of the listed symptoms appear on the skin, you should consult a dermatologist to accurately determine the type of disease.
Sticking of eyelashes, one of the manifestations of demodicosis
Treatment regimens for demodicosis: how to reduce the activity of skin demodex mites even without drugs
What is demodicosis is the first question asked by teenagers or adults with acne at an appointment with a dermatologist.
This rash has the character of rosacea - inflammatory elements above the surface of the skin. The color is bright red. Pathology is caused by Demodex skin mites. There are two types of pathogens that can be transmitted from dogs through feather pillows:
- D. Follicullorum – affects the eyelash bulbs, causes demodectic blepharitis,
- D. Brevis is a mite that feeds on the secretions of the sebaceous glands.
Symptoms
A rosacea-type rash appears on the face - these are large red coals. If there are a lot of mites, then convex granulomas are formed. They do not itch and do not bother a person. But the number of acne continues to increase, the skin becomes lumpy and greasy. Vascular networks and capillaries expand.
The longer mites live and reproduce, the more greasy the skin becomes. Against the backdrop of a long life of demodex without treatment of the pathology, an allergic component is added over time, which increases swelling and redness. A vicious circle is formed.
In men with demodicosis, the problem of rhinophyma . This is an inflammatory lesion of the skin of the nose with hypertrophy of all elements. Before the appearance of rhinophyma, demodicosis developed in the skin for several years.
Demodicosis of the head is a rare pathology that often develops against the background of seborrhea and is characterized by hair loss, flaking and the appearance of dandruff, itching of the scalp.
Interestingly, the demodex mite can live quietly in small numbers in the human epidermis, that is, on the top layer of skin. It does no harm and feeds on dead cells.
Ticks can be picked up from dogs. German shepherds and French bulldogs are often affected by it. But toy terriers and cocker spaniels do not suffer from this pathology. Demodicosis is also transmitted from an infected person through close household contact and the use of pillows and shared towels.
If demodex is localized on the edge of the eyelids, then the symptoms are as follows:
- sensation of a foreign object in the eye,
- redness and irritation of the eyelids,
- sticking and loss of eyelashes followed by abnormal growth,
- eye fatigue.
Read more about demodectic blepharitis here.
If the human body begins to produce more sebum, then there is a risk of demodicosis becoming more active. An exacerbation of the pathology is observed in the autumn-winter period, when the nonspecific resistance of the skin decreases. Hormonal changes in the body, especially local hormonal ointments, can provoke demodicosis.
Photo
perioral demodicosis of the face photo Photo of treatment of demodex Photo of demodicosis of the face Rhinophyma with demodicosis Demodectic mange of the eyelids photo Demodectic mange of the scalp photo
Diagnostics
Tests for demodicosis must be taken prepared. To do this, 3 days before the analysis, it is recommended to stop using any cosmetics, wash your face with clean running water and not use cream.
Then the dermatologist scrapes the facial skin in several places. The scraping is examined under a microscope, the analysis does not take more than 10 minutes. The diagnosis is made when more than 5 mites per 1 cm² are found on the skin . If there are fewer ticks, then a carrier diagnosis is made.
4 eyelashes from each eyelid for analysis and examine the hair follicle under a microscope. The diagnosis is made if more than 4-5 parasites were identified during the examination.
Treatment
To treat demodicosis, it is necessary to find out the reason for the increase in sebum production and try to stop it. If you do this, the tick will stop getting enough food and the pathology will disappear on its own. But in most cases, combined treatment of demodicosis is used with the use of drugs and proper daily hygiene.
Hygiene rules if you are concerned about demodicosis on the face:
- hygiene procedures should be carried out with disposable napkins, not towels,
- hats and scarves are supposed to be washed every 3 days,
- it is necessary to change the pillowcase on the pillow and, if possible, other bedding accessories daily,
- you need to wipe your glasses with alcohol wipes every day,
- you need to replace the natural filling of the pillows with padding polyester,
- avoid allergenic cosmetics,
- check pets for tick carriers.
All drugs that are sold to treat demodicosis must have a drying and anti-inflammatory effect. They use products in the form of demodicosis creams and ointments to disinfect the skin. On average, the treatment period for demodicosis is 2 to 3 months.
For demodicosis of the eyes, stop Demodex drops are used for treatment. Ointments and creams used are Dermazol, Demalan, Blefarogel No. 2. Read more about the treatment of demodicosis of the eyelids or eyes in this article.
Diet for demodicosis
The main treatment method is a diet for demodicosis. It is the main one, since nutrition directly affects the oiliness of the skin and the amount of sebum secreted. Products that increase sebum production:
- sweets in any form (easily digestible carbohydrates),
- carbonated sweet drinks,
- spicy food,
- cocoa, chocolate and coffee,
- fatty foods, fast food and offal (sausages, sausages).
It is necessary to normalize the intake of vitamins, give preference to fresh fruits and vegetables, lean meats. The diet should be filled with cereals.
Until the patient gives up junk food, demodicosis cannot be completely cured with the help of medications. The mite will multiply in the secreted fat.
Drugs
Facial demodicosis is treated comprehensively. There is no need to prescribe antibacterial drugs or antibiotics to the patient. This is necessary only against the background of the addition of bacterial flora. In this case, erythromycin is prescribed in a short course of up to 10-15 days.
demodicosis talkers on a regular basis. One of the components of the mash is boric alcohol, which dries out the skin. But he will be able to stop the development of demodicosis only in the first 2-3 weeks.
It is not recommended to take metronidazole tablets. They have a toxic effect and can reduce the body's reactivity (immunity). The products will not work on mites living on the skin.
Preparations based on cis-retinoic acid – dry the skin well . But they have many side effects that are caused by hypervitaminosis of vitamin A. The drugs are prescribed for advanced demodicosis by dermatologists.
External remedies and ointments for demodicosis
Sulfur ointment for demodicosis is used because of its acaricidal (ability to kill ticks) and antiseptic effects. Apply to the affected areas of the skin and rub in thoroughly for 5 days.
Ivermectin and a drug based on it, Solantra, are an acaricidal agent that can kill ticks and is used in the form of a cream or gel. The cream is applied once a day for 4 months.
Tar soap effectively helps to cope with mites on the skin You can make a mask from zinc paste and birch tar - once a day, keep it on for at least an hour. Apply daily for several weeks.
To treat accompanying acne, you can use Rosamet cream for demodicosis. It is made on the basis of metronidazole. It is worth applying the cream 2 times a day, but use it only if previous medications are ineffective.
Recipe for external and complex treatment of demodicosis: Rosamet cream + compress of Dimexide with water (1:3) for 15 minutes, then rinse off + skin mask made from a mixture of zinc ointment and birch tar: 4 drops of tar are needed per teaspoon of ointment.
Other schemes and folk methods
All plants, in the process of natural protection against parasites, produce phytoncides, which are converted into hydrolates. These substances are harmful to bacteria, viruses, and mites. For demodicosis of the face and eyes, you can use natural hydrosols: chamomile, wormwood, linden, lavender, calendula, mint, rose.
With these products you can make therapeutic compresses. It is necessary to prepare a decoction or infusion of these plants, then soak a cotton pad or gauze in it and apply it to the face for 15 minutes.
Loading…
Source: https://prof-medstail.ru/bolezni/shemy-lecheniya-demodekoza-kak-snizit-aktivnost-kozhnogo-kleshha-demodeksa-dazhe-bez-preparatov
Forms of demodicosis of the skin
Demodicosis does not always manifest itself in the same way; sometimes the disease is complicated by certain factors. There are several forms of demodicosis.
- Erythematous-squamous demodicosis. Its symptoms are redness, peeling of the skin, the formation of scales and small papules.
- Papular demodicosis. Appears as large red papules.
- Papulopustular demodicosis. Blisters filled with pus (pustules) appear on the skin.
- Rosacea-like demodicosis. The external manifestations are similar to the disease rosacea - rosacea appears on the skin.
- Combined demodicosis. The most common form. Manifestations of all forms of demodicosis occur on the affected skin.
If you do not pay attention to the problem in time and do not start treatment, or try to deal with the manifestations of demodicosis on your own, you can get serious complications.
Rosacea-like demodicosis manifests itself as rosacea
Prevention of re-infection
It is possible that after completing the course, re-infection will occur.
Typically, allergic manifestations disappear after discontinuation of use. Otherwise, you should immediately call a doctor.
To prevent relapse, you must:
- Observe the dosage and frequency of use of the ointment (if the doctor told you to use it 3 times a day, then apply it no more often or less often).
- During treatment, the patient must observe the rules of personal hygiene: take a shower regularly, wash your face, and do not touch the skin (especially infected parts of the face) with dirty hands.
- It is recommended to avoid cosmetics and products that can harm inflamed skin or clog pores (powder, concealer, foundation).
- During treatment, be sure to change towels, bed linen and underwear frequently. It is advisable to do this daily - parasites may remain on underwear and clothes, which can again end up on the face. Removed clothing and underwear should be washed immediately.
After completing the course, it is advisable to undergo a re-analysis. It is also recommended to take the test another 1-2 weeks after the end of treatment to make sure that the mite has not reappeared in the skin from the remaining eggs.
Diagnosis of demodicosis
Diagnosis of demodicosis is carried out in dermatovenerological clinics. First of all, scraping is done from the affected surface of the skin. If demodex mites are found, a diagnosis of demodicosis is made. Additional research is being conducted to select an effective treatment method.
- Blood tests (general, biochemical, glucose).
- Immunogram.
- Bacteriological culture of the nasopharynx.
- Stool analysis.
- Microscopic examination of fluid from sebaceous ducts and pustules.
Based on the results of clinical studies, the doctor makes a prognosis and prescribes a treatment plan.
Treatment regimen for facial demodicosis
In therapy, good results are achieved using a stepwise approach:
- The “foundation” of treatment is a balanced diet. The patient should eat portions of fruits, vegetables, proteins, and “good fats” each day.
- Stage 1 – daily use of special dermis care products. The medicinal and cosmetic gels “Demoten” and “Anti-cuperose” are recommended.
- The 2nd stage includes local therapy. The doctor prescribes antibacterial and antiprotozoal drugs: Elidel, Tacrolimus.
- Stage 3 – systemic therapy. Antibacterial drugs (Doxycycline), antiprotozoal drugs (Ornidazole) and retinoids (Isotretinoin) are prescribed.
Be sure to read:
What is demodex: treatment at home, causes and symptoms
The disease causes dry skin. To restore the level of hydration, Locobase and Pantoderm are used.
How is demodicosis treated?
Therapy for almost every skin condition must perform several tasks simultaneously. Demodectic mange is no exception. Therapy has several directions.
- Removal of the infecting agent (mite).
- Removing a concomitant infection if it appears (bacterial or fungal).
- Restoration of the skin and its normal functions.
- Increased immune strength.
To achieve the goals, drug and hardware treatment, as well as vitamin therapy, are used. The remedy for demodicosis should be selected by a doctor; it is advisable to consult a dermatologist and dermacosmetologist.
To make a diagnosis, you should consult a dermatologist
Drug therapy for demodicosis
Using a whole range of medications will help you completely get rid of demodicosis and its external manifestations.
- Acaricidal preparations for demodicosis. Destroy demodex. These are mainly ointments for external local use - benzyl benzoate, zinc, sulfur, ichthyol, permethrin, aversectin ointments, products with metronidazole.
- Local antibiotics. Gels are usually prescribed and applied to the affected areas of the skin.
- Keratolytics. Products that cause exfoliation of dead epidermal cells. Improves the appearance of the skin. The most common keratolytic is salicylic acid.
- Immunomodulators.
Every year ticks become more and more resistant to existing drugs. Permethrin ointment is no longer very effective in fighting parasites and helps few people. Currently, pharmacological companies and research centers are developing new medicinal acaricides.
Ichthyol ointment, an acaricidal drug
About the principles of treatment
Experts believe that in pursuit of a quick effect, one should not forget about the danger of ending up with over-treated skin. Complete removal of the tick leads to an imbalance of the natural microflora on the face, damage to the protective barrier, and increased skin sensitivity. Treatment must be comprehensive and comprehensive, taking into account all existing associated problems in the body.
You may also be interested in: Treatment of parasites: how to use the drug Intoxic
What principles should therapy be based on:
- prescription of systemic drugs orally (Trichopol);
- local exposure to traditional acaricides (Benzyl benzoate, Sulfur ointment, Permethrin, etc.) and drugs based on azelaic acid (for example, Skinoren);
- treatment of all foci of chronic infection in the body;
- using sunscreen before going outside;
- diet – exclude alcohol, fast food, sweets, hot drinks, fatty foods;
- proper organization of daily facial skin care - exclude all oil-based cosmetics;
- competent and mandatory washing in the morning and evening before applying medications to the skin.
Good sustainable results can only be achieved by combining all of the above points for 1.5-2 months. The treatment regimen for demodicosis is selected individually in each case. An important condition is a thorough collection of anamnesis in order to accurately establish the cause of the development of demodicosis and the involvement of doctors of different specialties to help the patient if necessary (gynecologist, endocrinologist, gastroenterologist, etc.).
Vitamin therapy for demodicosis
Vitamins are low molecular weight compounds that have strong biological activity. These substances are involved in the regulation of all functions of organs, tissues and cells. Vitamins for demodicosis help improve the overall condition of the skin and increase the body's resistance to infection.
- Group A. Vitamins that dissolve in fats easily penetrate cell membranes. Affect the growth of the body. Vitamin deficiency leads to dry skin and the appearance of acne. The vitamin is found in fish oil, pork and beef liver, butter, spinach and lettuce leaves, and green onions. You can buy fish oil in gelatin capsules at the pharmacy.
- Group B. Belong to water-soluble vitamins. Contained in liver, cereals (buckwheat, rice, millet), beans and potatoes.
- B1 (thiamine) – regulates carbohydrate metabolism, maintains normal functioning of the heart and nervous system.
- B2 (riboflavin) – regulates cell division processes and protein metabolism.
- B5 (pantothenic acid) - takes part in oxidation reactions, metabolism of proteins, fats and carbohydrates, synthesis of fatty acids (components of cell membranes).
- B6 (pyridoxine) – is involved in the regulation of metabolic processes and hematopoiesis.
- B12 (cyanocobalamin) – has the highest biological activity in its group. Participates in the processes of hematopoiesis, in the synthesis of amino acids and other compounds important for the body.
- Vitamin C (ascorbic acid). Participates in the body's redox reactions, is a strong antioxidant, and improves immunity. Contained in vegetables and fruits.
- Vitamin E (tocopherol). Fat-soluble vitamin. Works in cell membranes, is an antioxidant (its effect is enhanced by vitamin C). Contained in vegetable oils.
Vitamin therapy helps normalize the condition of the skin and ensure its renewal. When treating demodicosis, tableted vitamin complexes or a special diet are prescribed.
Tocopherol (vitamin E) is found in vegetable oils
CAUSES AND SYMPTOMS OF DEMODECOSIS
Mites can live in the roots of facial hair and eyelashes.
At risk are adolescents at the time of puberty, pregnant women, as well as those suffering from gastrointestinal diseases and those who have suffered stress.
Children before puberty are not at risk of the disease due to the insignificant activity of the sebaceous glands. After all, parasites feed on sebum: if there is little of it, the demodex (or “ironite”) has nothing to eat.
Demodicosis occurs as follows:
- The functioning of the sebaceous glands is disrupted.
- The quality and quantity of sebum changes.
- A microflora favorable for ticks is formed.
| HORMONAL DISBALANCE |
|
| GASTROINTESTINAL DISEASES |
|
| SEVERE STRESS | |
Symptoms of demodicosis
- Rash, pustules on the face or décolleté;
- Itching and discomfort;
- Lumps and ulcers on the face;
- Shine in the T-zone;
- Plaque in the eyelid area;
- Brittle and loss of eyelashes;
- Pale or purple complexion in advanced conditions.
We recommend: WHICH PEELING IS BETTER FOR REJUVENATION: 9 recipes after 30 years
Precautionary measures
To identify the disease, it is necessary to conduct the following examinations:
Tests for demodicosis (Table)
| WOMEN | FOR MEN |
| Blood for hormones (gynecologist-endocrinologist) | Blood for hormones (endocrinologist) |
| Gynecological ultrasound | |
| |
In some cases, you also need to be tested for antibodies to thyroglobulin and have a gastroscopy.
Diseases with similar symptoms
Initially, it is necessary to correctly diagnose the problem in order to choose the right treatment strategy. It is important not to confuse with similar dermatological problems:
- Rosacea (papules),
- Folliculitis,
- Dermatitis,
- Spider veins,
- Fungal diseases
- Allergy.
Most often, acne and oily seborrhea are diagnosed simultaneously with demodicosis.
20 prohibitions for demodicosis (Table)
Even if there are no problems with the gastrointestinal tract, it is important to follow a diet and other restrictions during the treatment process.
EVERYTHING IS “NO” FOR DEMODECOSIS:
| IN NUTRITION |
|
| ON A REST |
|
| IN MAKEUP |
|
| IN CARE |
|
| FOR THE NIGHT |
|
The diet should include plenty of fruits and vegetables, Omega-3 and Omega-6 fatty acids (found in seafood).
We wash ourselves only with hydrophilic oil, foams or soft gel-like products. No alcohol or soap to maintain proper skin acidity.
Frequent washing with demodicosis will be harmful, so during the day it is better to use damp matting wipes.
Hardware treatment of demodicosis. Cryotherapy
Hardware treatment effectively removes manifestations of demodicosis. The most common way to combat the disease is cryotherapy. The method uses liquid nitrogen. In the clinic, an applicator that releases gas vapor is used to treat the affected areas of the skin using rotational movements. The procedure is repeated twice every ten minutes. Damaged surfaces are treated until the skin turns slightly white. After such cryomassage, persistent redness appears.
A more comfortable and advanced way to combat the manifestations of demodicosis is the action of a nitrogen-air jet. The method is softer, the skin is practically not injured. You can adjust the temperature of the gas mixture.
Cryopilling and cryodermabrasion
In addition to cryomassage, cryopilling and cryodermabrasion are performed. These are methods of cleansing the face from dead and rough skin.
For a full course of treatment of demodicosis, more than 10 cryotherapy procedures are needed.
Physiotherapeutic procedures can also be used to treat demodicosis, but only as prescribed by a doctor. The following types of physiotherapy are suitable for this type of dermatosis:
- UHF, the action of a high frequency electromagnetic field on the skin,
- UV - irradiation,
- laser therapy.
Physiotherapy aims to improve the condition and natural functions of the skin.
To eliminate demodicosis you need at least 10 cryopilling procedures
About skin care
With demodicosis, not only does the amount of sebum increase, but its qualitative characteristics also change, for example:
- bactericidal properties decrease;
- PH changes to the alkaline side;
- natural hydration decreases.
Therefore, in the complex treatment of demodicosis, it is very important to use sebum-regulating agents that help reduce the amount of sebum, as well as acids to restore normal skin reaction and achieve a keratolytic effect.
What not to do with demodicosis:
- visit solariums, baths and saunas, take hot baths for the face;
- use fatty creams and oils, various nourishing masks that feed ticks;
- squeeze out pimples and blackheads with your hands;
- do facial massage;
- use decorative cosmetics, foundation, compact powder, cream powder (loose powder can be used occasionally);
- apply a facial scrub during treatment;
- go to bed without cleansing your face - cosmetics should be washed off with warm water along with dust, sebum and exfoliated epithelium, so as not to feed the tick at night.
It will also be interesting: What drugs exist for roundworms?
What can be done for demodicosis in a cosmetologist’s office:
- cryomassage with liquid nitrogen (this is better than just using ice at home) - usually carried out towards the end of the main therapy, several courses will help get rid of the tick, relieve inflammation and improve skin microcirculation;
- cryosauna – increases immunity, but a doctor should tell you about contraindications;
- the use of chemical facial skin cleansers (salicylic, pyruvic, almond procedures) - such peeling for demodicosis is used after or at the end of treatment to correct traces of the disease and prevent relapses, it has an anti-inflammatory effect, reduces sebum secretion, and narrows pores.
What to do at home:
- wash your face in the morning and before bed with water at room temperature or acid washes with AHA (glycolic acid) and BHA acids;
- wipe your face with ice every day, better in the morning instead of washing your face - ice can be made from herbal infusions (parsley, calendula) or cucumber juice;
- make moisturizing masks (gel masks) 1-3 times a week.