Eversion of the century
– cicatricial deformation, which not only creates an aesthetic defect, but also brings physical discomfort to the patient.
Eversion of the eyelids can occur for various reasons, but surgery is almost always necessary to correct this problem. Natalia Alekseevna Vaganova
to talk in more detail about the methods of surgical correction for eversion of the eyelid .
Corr:
Natalia Alekseevna, what reasons can lead to eversion of the eyelids?
Eversion of the eyelids can be post-burn, post-traumatic and post-operative.
.
Corr:
Are the treatments different in these cases or are they independent of the underlying causes?
Surgical treatment is approximately the same everywhere. Let's start with a post-burn case. Let's say we have an inversion of the lower eyelids. At the beginning of the operation, three silk holders are placed on the lower eyelid, then the eyelid is freed from scars with slow movements of the scalpel. At the same time, our wound increases. When the lower eyelid is freed from scars, it is fixed in a state of hypercorrection. In fact, the lower eyelid is sutured to the eyebrow area. The second stage is the collection of donor tissue. Typically the donor area is the inner surface of the shoulder. For eyelids it is suitable for the texture and quality of the skin. The graft is taken using semilunar incisions, placed on the lower eyelid and fixed to the edge of the wound. Apply a bandage with chlorhexidine to the wound. The donor wound is also sutured, a chlorhexidine pad is applied and bandaged.
Corr:
Can the patient go home after this? How does the recovery period proceed?
The patient wears the bandages for 6 days. On the 7th day the sutures are removed. First, we simply cut off the fixing sutures and see if the grafts have taken root. As a rule, they take root. During this period, a retraction process occurs - the skin contracts. But we keep the stitches in place for another 1-2 days. We remove them only for 8-9 days. During this period, it is useful to use various physical procedures: magnetic therapy, ultrasound, microcurrents.
Corr:
What if the upper eyelid was damaged?
Aesthetic indications for blepharoplasty
Blepharoplasty solves the following problems:
- excessive sagging of the skin of the upper eyelid;
- hernias of the lower eyelids - so-called bags under the eyes. This is a layer of fatty tissue accumulated in one place. Due to age or genetics, connective tissue septa cease to hold the lipid layer, and it begins to bulge;
- drooping corners of the eyes;
- eye asymmetry;
- sprain of the orbicularis oculi muscle;
- blepharochalasis - skin atrophy, as a result of which small wrinkled folds form above the eyelid;
- exophthalmos - excessive protrusion of the eyeball, bulging eyes;
- epicanthus - an additional fold at the inner corner of the eyelid (“Mongolian fold”).
If necessary, the plastic surgeon can slightly change the shape of the eyes.
Contraindications to blepharoplasty
Blepharoplasty is a fairly simple procedure, so it has few contraindications. Due to the fact that the operation is performed under local anesthesia and takes less than an hour, it can be performed even on elderly people without fear that it will somehow negatively affect their health.
Blepharoplasty of the upper eyelids is often performed not only for aesthetic, but also for functional reasons, for example, in cases where a drooping eyelid contributes to poor vision or eyelashes begin to scratch the cornea, leading to inflammatory processes. Blepharoplasty of the lower eyelids, on the contrary, in most cases pursues an aesthetic goal: to remove bags under the eyes, to get rid of so-called “fatty hernias,” wrinkles, and excess skin under the eyes. However, contraindications for any type of blepharoplasty are the same; below we will consider them in more detail.
- Absolute contraindications to eyelid blepharoplasty are:
- serious diseases of internal organs;
- human immunodeficiency syndrome (AIDS);
- malignant tumors (oncological diseases);
- blood clotting disorder;
- high blood pressure;
- diabetes mellitus II-III degree;
- diseases of the cardiovascular system and other serious diseases of internal organs;
- hyperfunction and other diseases of the thyroid gland;
- increased intraocular pressure;
- the patient has infectious diseases of the orbital region;
- dry eye syndrome;
- exacerbation of chronic diseases;
- acute respiratory infections;
- menstruation (at least 4 days must pass before and after menstruation).
Before blepharoplasty, the surgeon prescribes a preoperative examination and standard tests, as with any other surgical intervention. This is a general blood test, a blood test for HIV, RW (syphilis) and the Australian antigen HBS, HSV (hepatitis B, C). This is a necessary procedure in order to find out about the patient’s health status and find out whether the patient has any contraindications for the use of intravenous (general) or local anesthesia. Based on the results of the examination, the surgeon decides whether the patient can undergo blepharoplasty or not.
In addition, it should be remembered that two weeks before eyelid blepharoplasty surgery, the patient is contraindicated from insolation (tanning), drinking alcoholic beverages and spicy food, and smoking at this time is also extremely undesirable. After blepharoplasty, eye strain is contraindicated, for example, working at a computer and direct sunlight - it is recommended to wear smoked glasses and try to treat the area around the eyes as carefully as possible. You can apply makeup to your eyelids in 10-14 days, and full recovery will occur in a couple of months.
Medical indications for blepharoplasty
An ophthalmologist will send you for reconstructive blepharoplasty if it is determined that the structure of the eyelids interferes with the functioning of the visual apparatus. Indications may be:
- ptosis of the upper eyelid - its abnormally low location;
- severe narrowing of peripheral vision due to excessive overhang of skin folds;
- entropion - inversion of the eyelid, when the eyelashes and its edge are turned towards the eyeball;
- ectropion - inversion of the tissues of the lower and upper eyelids outward.
Blepharoplasty has moved into the arsenal of plastic surgeons from ophthalmology, where similar interventions were carried out back in the century before last. However, modern technologies have made it possible to classify blepharoplasty as a one-day operation: after it, the patient can return home the next day.
Is blepharoplasty losing ground to new techniques?
New gentle technologies for comprehensive rejuvenation of the eye area offer an exceptional expansion of the rejuvenating effect of blepharoplasty, a traditional method of local eyelid plastic surgery.
New technologies of vertical face lifting, one of the stages of which is blepharoplasty, are the best option for those who need a more complete, natural and long-term effect of facial rejuvenation without a total operation of a circular SMAS lift and long rehabilitation.
Nine out of ten patients of the DoctorPlastic clinic, who during the consultation learn about the new possibilities of modern “vertical” facial plastic technologies, change their decision and instead of classic blepharoplasty, undergo one of the complex vertical lifting operations.
The reasons for this are obvious - complex plastic surgeries provide a fundamentally better rejuvenating effect, without requiring additional incisions and practically without increasing the invasiveness of the surgical procedure. This is how Professor Samuelsson (a well-known European specialist, president of the Swedish Association of Plastic Surgeons, practicing at the Moscow DoctorPlastic clinic) comments on these statistics:
| – Classic blepharoplasty is an operation limited to the area of the upper or lower eyelids, in most cases it cannot completely solve the problem of rejuvenation of the upper eyelids. This is very easy to understand if you consider the fact that one of the reasons for ptosis of the upper eyelids, which the patient wants to get rid of, is age-related changes in the tissues of the forehead and eyebrows. The problem of rejuvenating the lower eyelids and correcting bags under the eyes is usually directly related to the presence of age-related changes in the midface, and not only with the aging of the skin of the lower eyelids and the formation of fatty hernias. Therefore, lifting the tissues of the midface area is the most important part of the rejuvenation of this area, without which it is impossible to obtain a natural and complete result. |
Let's do a little experiment. Stand in front of a mirror and slightly raise your eyebrows with your fingers. Do you see how the upper eyelid has lifted and smoothed out, and the look has become more open? This is exactly the effect that eyebrow lifting can achieve in combination with upper blepharoplasty.
Moreover, this operation does not require additional incisions. All necessary manipulations: lifting the forehead, eyebrows and correction of the upper eyelids are carried out through single incisions in the fold of the upper eyelid. Exactly the same as those done during classic blepharoplasty.
But if such incisions are made, eyebrow ptosis is present, it’s simply stupid not to tighten the eyebrows along with the eyelids!
Dr. Igor Anatolyevich Bely, a leading surgeon in the department of facial plastic surgery, can offer patients of the DoctorPlastic clinic his own modification of the transpalpebral method of comprehensive rejuvenation of the upper face, including forehead lift, eyebrow shape correction and upper eyelid surgery.
The effect of such an operation corresponds to the total result of two separate surgical interventions - endoscopic forehead lift and upper blepharoplasty. At the same time, this technique has a number of obvious advantages, the main of which are:
- minimum incisions (complete absence of scars in the scalp and temples);
- significantly less traumatic;
- shorter and easier rehabilitation;
- minimal risk of surgical complications.
Doctor of Medical Sciences, Professor Bely notes another important advantage of this technique. The unique surgical instrument he uses, which is made according to the doctor’s drawings in a single copy, allows you to very accurately model the line of the eyebrows, achieving a beautiful bend without the unnatural “upturnedness” that often gives away the plastic surgery performed.
When planning rejuvenation of the infraorbital area, do not rush into lower blepharoplasty. This is not the only and not always the best opportunity to rejuvenate this area that modern plastic surgery can offer!
Now let's look at the reasons for age-related changes in the molar zone of the face and lower eyelids. Obviously, the problems in this area are associated with aging and ptosis (drooping) of the tissues located below. Aging and the “sliding” of the soft tissues of the cheekbones and cheeks contribute to the formation of circles under the eyes and nasolabial folds. Obviously, in this case, lower blepharoplasty cannot completely solve the problem of rejuvenation without correcting the underlying area of the face.
In order to obtain the most complete and natural rejuvenating effect, it is necessary, along with the correction of the lower eyelids, to return the tissues that have sagged with age to their original state. The best option for such a correction is check-lifting (lifting the midface area) and lower blepharoplasty combined with it. Both procedures are performed through a single incision that runs along the edge of the eyelid, along the eyelash line (as with traditional blepharoplasty).
An important advantage of this complex method is that the lifting occurs strictly vertically, from bottom to top. This allows the tissue to be returned exactly to its original position, without moving it to the periphery, which gives an extremely natural result that cannot be achieved using other methods of mid-zone lifting.
Check-lifting in combination with lower eyelid surgery provides the most complete, natural and lasting rejuvenating result without additional incisions. As an additional valuable bonus, patients receive correction of nasolabial folds. This complex plastic surgery is so easy to tolerate that it is usually performed on an outpatient basis, under local anesthesia.
Modern facelift techniques offered by DoctorPlastic clinic specialists are the best choice for those who strive for maximum results, but are not ready for scars and do not want to spend several months on rehabilitation.
Plastic surgeries are performed by world-class specialists: Professor of Medicine, MD, President of the Swedish Association of Plastic Surgeons Ulf Samuelsson and Professor, Doctor of Medical Sciences, one of the best Russian specialists in the field of facial plastic surgery - Dr. Bely. You can find out more about specialists and methods on the clinic’s website: www.doctorplastic.ru.
Before and after surgery: photos
Types of blepharoplasty
Tell the surgeon in detail about your expectations from permanent blepharoplasty - the doctor will take into account your anatomical features and select the optimal surgical technique. All classical technologies involve incisions with a surgical scalpel.
Upper or anchor blepharoplasty
Upper eyelid blepharoplasty is the most popular operation. Aimed at removing excess skin, fat or muscle in this area. An experienced VIP Academy surgeon will determine how much tissue needs to be excised so that the eyelids can close properly.
Lower, or subliciary, blepharoplasty
Blepharoplasty of the lower eyelid involves excision of fat bags under the eyes, and, if necessary, the skin stretched over them is removed. Sometimes the desired effect is achieved through the redistribution of fat depots.
Circular blepharoplasty
This is a simultaneous lift of the upper and lower eyelids. It takes place in several stages, lasts longer than other operations (up to 3 hours) and is considered more complex. The technique involves a highly qualified surgeon; the maximum number of defects is eliminated at a time.
Transconjunctival blepharoplasty
The surgeon can make an incision above the upper eyelashes, on the outside of the eyelid, or mini-punctures on the mucous membrane, on the inside. In the latter case, the technology is called transconjunctival. This type of blepharoplasty allows you to achieve a high aesthetic effect, since no stitches are needed at all, which means there will be no scars.
Sometimes eyelid blepharoplasty alone is not enough to correct the defect. It is combined with a surgical facelift in certain areas (frontal, superciliary, infraorbital, zygomatic or cheek areas).
Types of blepharoplasty: assessing the effectiveness of non-surgical and surgical methods
Wrinkles, bags and ptosis can be eliminated using both surgical and conservative methods. Surgery is not the only option to restore your eyelids to their former elasticity and make your eyes more open. If the changes are minimal, then think about alternative methods of eyelid skin rejuvenation - there are a lot of them. Here are some alternatives to surgical eyelid surgery that will help in the early stages of age-related changes:
- botulinum toxin injections (Botox, Dysport). They allow you to remove facial wrinkles around the eyes;
- mesotherapy or biorevitalization. Using a fine needle, a specialist introduces special cocktails enriched with vitamins, microelements and other biologically active components, which simultaneously increase skin moisture and turgor and smooth out fine wrinkles;
- RF – lifting, or thermolifting, thermage. High-frequency radio waves entering the tissue heat the collagen fibers contained in the subcutaneous layer. This protein folds, and the body has to form new protein molecules, which results in a rejuvenating effect. In other words, the process of tissue regeneration is artificially provoked. The name of the procedure may change depending on the name of the equipment the cosmetologist uses, but the method is the same in all situations;
- Ultrasonic lifting is the effect of ultrasound, which causes collagen fibers to become denser and stronger. The procedure allows you to obtain a noticeable tightening effect;
- laser rejuvenation. Laser beams evaporate specific layers of the skin, forcing the body to urgently start their restoration.
We recommend: How is forehead blepharoplasty performed?
The effectiveness of non-surgical methods is limited. And sooner or later, those who want to preserve their youth, if they do not want to put up with the current state of affairs, resort to surgical methods of eyelid lifting. The operation will have to be done by those people who want to change the shape of their eyes.
You should not be afraid of such an intervention - techniques are constantly being improved, and today it is no longer such a traumatic intervention as it was 10 years ago. For example, if it is necessary to remove fatty hernias, transconjunctival blepharoplasty is used, in which an incision is made on the inside of the eyelid.
There are no visible traces of such an operation. In traditional blepharoplasty, an incision is made along the lower eyelash line (for lower eyelid surgery) or along a natural skin fold (for upper eyelid surgery). Therefore, postoperative scars will be completely invisible.
Examination before blepharoplasty
Before blepharoplasty, it is necessary to undergo an examination to determine contraindications to surgery. Mandatory manipulations include:
- general blood and urine tests,
- blood chemistry,
- coagulogram - test for blood clotting,
- tests for HIV, syphilis, hepatitis B and C,
- ECG.
At the VIP Academy, patients must be examined by an ophthalmologist, because blepharoplasty is contraindicated for keratitis, blepharitis, glaucoma, and cataracts.
How is the operation performed?
The surgeon will treat the eyelids with an antiseptic solution three times, then will delimit the surgical field from the surrounding tissues with sterile material.
Injections of local anesthetic are the only painful part during surgery. While the medicine is being administered, you will feel pain and swelling of the soft tissues of the eyelid. Unpleasant symptoms will be replaced by complete insensitivity within 1–3 minutes.
Upper blepharoplasty
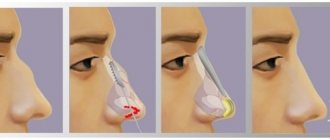
The surgeon will mark the skin of the upper eyelids and mark the incision lines. In upper eyelid blepharoplasty, the tissue is cut 7–9 mm from its edge and excess skin is carefully excised.
Capillary bleeding is stopped with an electrocoagulator - a device for cauterizing damaged vessels. A competent surgeon begins suturing the wound only after the bleeding has sufficiently stopped. Sutures are placed on the upper eyelid with a thin atraumatic needle strictly along the incision line.
Lower blepharoplasty
In lower eyelid blepharoplasty, the incision is made at a distance of 2–3 mm from the ciliary edge.
The skin of the lower eyelid, together with the orbicularis oculi muscle, is carefully moved down a few millimeters, opening access to the hernial sacs. They are excised, after which the skin of the lower eyelids is returned to its original position.
The surgeon excises excess skin folds near the primary incision with a single linear flap.
The last stage of lower blepharoplasty is layer-by-layer suturing of the wound of the lower eyelids. The suture is placed intradermally to avoid scarring and poor alignment of the wound edges. Our surgeons apply cosmetic sutures using modern techniques and achieve high aesthetics.
Methods of lower eyelid blepharoplasty
There are two ways to perform blepharoplasty:
- Classic lower eyelid surgery
When performing classic lower eyelid surgery, the incision is made along the natural folds, slightly away from the eyelash edge. This manipulation is necessary in order to open access to the localization of fat packets, to the orbicularis oculi muscle. Next, the surgeon delicately peels the skin away from the muscle and removes or redistributes the fatty hernias. If necessary, excess skin is excised. At the end of the operation, a cosmetic suture is placed on the incision area. During surgery, canthopexy is often performed to prevent cicatricial ectropion of the lower eyelid after blepharoplasty. This is required in particular for those patients who have a flabby eyelid edge.
The duration of the entire operation for lower eyelid blepharoplasty is about 1 hour.
Excision of the skin can also be carried out with a laser, but its use in the eye area is not recommended by many specialists
- Transconjunctival lower eyelid surgery
The transconjunctival method is most often indicated for young patients with slight excess skin of the lower eyelids. Transconjunctival blepharoplasty requires good, tight and elastic skin. The ideal patient is a young man or woman who does not have age-related changes, but has persistent and persistent bags under the eyes or swelling.
The advantage of the operation is that it is performed without an external incision. Access is through an incision or puncture in the conjunctiva of the eye. Then, excess fatty tissue is removed. No stitches are required as the mucous membrane heals very quickly. The operation also lasts about 1 hour. Read more about this technique here.
Gvaramia A.A. comments:
“Having performed eyelid surgery for more than 20 years, I can say with confidence that there is nothing better than a scalpel for this operation. I'm talking specifically about the skin incision. This is what I and most of my colleagues think. If a laser or radio knife is used, small vessels are “welded”: this is convenient for the surgeon, since the wound does not bleed. But this affects the quality of the scar! And for the best scar, I prefer a scalpel. The laser is a wonderful device, but its use must be appropriate in aesthetic medicine. Its use is justified in the transconjunctival technique, since the incision passes through the mucosa. But the final result in this case is not affected in any way by what exactly the doctor used to make the incision: it is solely a matter of the surgeon’s comfort.”
Rehabilitation
If you neglect the doctor’s recommendations during this period, the surgeon’s efforts may be in vain, and you will not get the desired effect. At first you will have to endure the inconvenience and show discipline.
The first hours after surgery
Within 3 to 4 hours after surgery, the anesthesia will wear off and you will feel mild pain in the eyelid area. You may also be concerned about:
- increased sensitivity to light,
- numbness of areas of the eyelid,
- double vision,
- increased tearfulness.
To relieve symptoms, your doctor will prescribe nonsteroidal anti-inflammatory drugs (NSAIDs). They also have an analgesic effect.
First week after surgery
On days 2–3, swelling of the soft tissues of the eyelid increases. It goes away on its own 5–7 days after blepharoplasty. Excessive swelling will help prevent simple rules:
- exclude from your diet foods that retain moisture in the body - salted, fried and smoked foods;
- reduce the amount of liquid consumed;
- avoid tilting your head and torso;
- do not engage in sports or physical labor;
- Avoid eye strain while reading, working at a computer screen or other gadgets.
These restrictions are lifted within 10–14 days after blepharoplasty. Until the wound on the eyelid has completely healed, you should not use decorative and caring cosmetics - the products can cause an allergic reaction or inflammation.
Sutures from the wound are removed on days 7–9 of the rehabilitation period.
Deferred period
The late rehabilitation period begins 2–3 weeks after blepharoplasty. At this time, the structure of the skin is gradually restored:
- swelling goes away completely;
- redness in the suture area disappears;
- new collagen fibers are formed.
The postoperative scar on the eyelids becomes invisible 1–2 months after blepharoplasty. At this time, you can already use cosmetics, so minor redness can be easily masked.
Consultation with a specialist:
Upper eyelid surgery is performed in much the same way. Holders are applied, the scars are removed, and a wound is formed. Then the upper eyelid is sutured to the cheekbone area. We collect skin from the inner surface of the shoulder and also stitch it up. The sutures are removed on the 7th day. If there was deformation of both the upper and lower eyelids, then usually one eyelid is done, and the other after 2-4 months.
Corr:
We looked at post-burn eyelid eversion. Let's talk about other cases.
Such correction can be attributed to both post-burn and post-traumatic deformities.
Corr:
What if a patient comes up with such a problem after undergoing blepharoplasty?
Such cases are rare. But if this has happened, and after the operation a cicatricial eversion of the eyelid appears, it needs to be eliminated. If this is discovered immediately after surgery, then we simply fix the lower eyelid in a state of hypercorrection, for example, with an adhesive plaster. As a rule, this only happens on the lower eyelid. The patient walks in this state for some time, and the inversion gradually disappears.
Corr:
What if a lot of time has passed since the operation?
Such cases are extremely rare. The correction is standard, as with post-burn deformities - a graft is transplanted. In general, patients who have inverted eyelids after blepharoplasty are prone to keloidosis. With such individual characteristics, the patient, before going for blepharoplasty, needs to look at: if there have been operations before, how postoperative scars behave. If there are keloid scars, then such patients should be treated with more caution.
Corr:
Let's now consider a general case. Let's say there is an injury to the eyelids. Should she be treated as quickly as possible?
In general, in the treatment of post-burn deformities there is an unspoken rule: if the patient has suffered burns, then it is most convenient to perform reconstructive operations a year later. The scars must mature. At the initial stage, when they are bright red in color, accompanied by itching and pain, the patient is treated with physiotherapy.
But in case of damage to the eyelids, they deviate slightly from this rule. Eyelids can be operated on earlier. For example, several months after the injury. The fact is that an open eyelid is a constant source of irritation. If the eye is open all the time, keratoses and diseases of the eye mucosa occur. Therefore, it is better not to delay treatment and have surgery early.
Natalia Alekseevna, thank you for your story! Cicatricial deformities are always unpleasant, and in the case of eyelids, it is also a matter of preserving vision. Therefore, we hope that a detailed discussion of this topic will be useful to our patients.
Possible complications
Most often, complications arise when the patient does not follow the doctor’s recommendations. But the surgical technique, the skill of the surgeon and the individual characteristics of the body are also of great importance.
What shouldn't scare you
Complications of blepharoplasty do not include pain and swelling - this is a physiological reaction of the body in response to trauma to the skin. After lower eyelid blepharoplasty, temporary lower eyelid separation is also possible. After 7–10 days, this phenomenon disappears, and the lower eyelid returns to its place.
What should you be wary of?
True postoperative complications include:
- hematoma formation - occurs if bleeding in the damaged tissues of the eyelid has not been sufficiently stopped;
- dry eye syndrome - tear production is impaired, the surface of the eye is not wetted by tear fluid;
- bacterial conjunctivitis;
- cysts on the suture lines;
- rough scarring of the wound - usually observed in patients prone to keloid formation. In them, any damage to the skin is accompanied by a violent reaction of the body in the form of proliferation of connective tissue.
Only some of the complications of blepharoplasty are considered to be surgical errors:
- violation of eye symmetry;
- eversion or drooping of the eyelid, incomplete closure - occurs when the surgical technique is violated, too large a musculocutaneous flap is excised;
- blindness is an extremely rare complication associated with the formation of a large hematoma in the retrobulbar space. Usually develops in the first hours after blepharoplasty
If you have any doubtful symptoms, contact your doctor immediately. The doctor will distinguish complications from the normal course of the postoperative period and prescribe therapy.
Contraindications
Complications of certain diseases of organs and systems may be contraindications. If the patient’s decision to operate remains unchanged, then careful preparation is carried out and a day for surgical correction is scheduled.
Contraindications may be temporary or absolute. In the first case, surgery is possible after eliminating the clinical situations; in the second, surgical manipulations are not possible.
When absolute contraindications exist, the patient can rely on alternative methods of correction.
The main ones include:
- aggravated medical history of the patient (serious pathologies of organs and systems);
- menstrual period in women;
- inflammatory diseases in the body of any etiology;
- increased intracranial pressure ;
- arterial hypertension ;
- dry eye syndrome;
- inflammation of the mucous membrane of the eye and soft tissues of the eyelid;
- diabetes mellitus (including decompensated treatment);
- oncological diseases of any localization;
- endocrine disorders (hypothyroidism, hyperthyroidism and others);
- hematological diseases;
- heart failure of varying severity;
- renal and liver failure (including replacement therapy).
Blepharoplasty is not able to eliminate some eyelid defects, for example, bags under the eyes, if the swelling is caused by a significant decrease in the excretory function of the kidneys and adrenal glands, or their pathological changes.
Before the operation, a number of medical examinations are carried out, including consultation with narrow and specialized specialists to exclude serious diseases.
The list of contraindications depends on the type of intervention.
Lower eyelids
Blepharoplasty of the lower eyelid is a gentle method of correcting the appearance of the periorbital area. It is used for pronounced age-related changes and is indicated for patients over 35 years of age.
On this topic
Other indications for using the method are congenital pathological and anatomical defects of the orbit that interfere with the normal visual process.
The main contraindications include the following patient conditions:
- intraocular pressure;
- hypertensive state;
- blood diseases and increased blood clotting;
- oncological formations of any localization;
- diabetes mellitus of varying degrees;
- “dry” syndrome due to insufficient functioning of the lacrimal glands;
- pathologies of the heart and blood vessels;
- increased secretion of the thyroid gland;
- menstrual bleeding (temporary contraindication).
The operation requires a special approach, since it affects a wide area of soft tissue along the lower edge of the eye. Before performing blepharoplasty of this type, other, less traumatic methods of surgery are always considered.
If alternative correction methods theoretically cannot lead to the desired effect, then a day of surgery is scheduled.
Upper eyelids
For this type of blepharoplasty, an external skin incision is made in the upper part of the eye, which is then hidden in the naturally formed crease of the eyelid. After a successful operation, such a suture is not visible upon visual inspection.
The main contraindications include:
- regular increase in intraocular pressure;
- diabetes mellitus in the terminal stage;
- thyroid dysfunction ;
- hypertensive diseases;
- heart disease and vascular pathologies;
- kidney, liver and respiratory diseases
- intolerance to anesthesia;
- disturbances in the functioning of the nervous system;
- infections, inflammatory processes in the body;
- inflammation of the conjunctiva of the eye.
Blepharoplasty of the upper eyelid may be impossible in case of injury and some pathologies of the anatomical structure.
Transconjunctival
Transconjunctival correction of the lower eyelids is a new method in blepharoplasty. The operation is performed by making an incision in the conjunctiva of the eye. Thanks to the method, soft and mucous tissues are not seriously damaged, vision is preserved, and the postoperative period is quite easy.
On this topic
The procedure is not possible for patients with the following pathologies:
- acute infectious and inflammatory diseases of the body;
- AIDS, other immunodeficiency conditions;
- menstrual bleeding in women;
- disturbances in the functioning of the hematopoietic and blood diseases;
- xerosis of the sclera of the eyes (dryness);
- oncological neoplasms of any etiology and localization;
- intraocular pressure;
- high blood pressure;
- endocrinological disorders.
Despite the ease of the operation, it is worth taking the preparation steps seriously and following all medical instructions.
Laser
The correction technique involves applying a laser to problem areas around the eyes. The procedure is not invasive, the risks of bleeding are eliminated, and the postoperative period is easier to bear.
On this topic
Laser correction is not suitable for all categories of patients:
- endocrine diseases, hormonal imbalances;
- diabetes mellitus of varying severity;
- infectious diseases;
- chronic inflammatory diseases in the acute stage;
- cancer tumors of any location;
- hematological diseases.
Laser blepharoplasty is one of the most gentle methods for correcting problems in the periorbital area. To ensure a successful operation and achieve maximum results, a thorough examination of the patient is carried out to determine the possibility of the procedure.
Result and forecast
The intermediate effect of blepharoplasty can be judged 2–3 weeks after surgery. The final result is assessed 3–6 months later and lasts 8–12 years.
But the skin continues to lose its elastic properties, so sometimes it may be necessary to repeat eyelid blepharoplasty ahead of schedule. In older age groups, it is often combined with a surgical facelift.
A good final effect from blepharoplasty is the result of a constructive dialogue between the doctor and the patient, the doctor’s skill and the correct rehabilitation period.
Recommendations after lower eyelid surgery
Even after plastic surgery is performed by a competent specialist, the result may be unsatisfactory due to the incorrect behavior of the person operated on.
One wrong action can reduce the efforts of a plastic surgeon to zero. In this regard, in order to properly complete the rehabilitation period, the following conditions must be observed:
- Wear sunglasses while on your face. They can not only protect your eyes from exposure to ultraviolet radiation, they will also protect them from branches and dust;
- exclude spicy and salty foods from the diet, which can cause increased swelling;
- Minimize physical effort: do not bend over, do not lift heavy things. Such actions will help avoid seam divergence;
- stop reading and watching TV;
- no smoking. Smoking can lead to vasospasm, which, in turn, will slow down tissue healing;
- It is recommended to sleep on your back, with the head of the bed raised. This will help reduce swelling after blepharoplasty.
If you were unable to avoid unpleasant consequences after surgery, there are a number of cosmetic and physiotherapeutic procedures:
- nourishing and moisturizing face masks that will help improve the condition of the eyelid skin;
- Lymphatic drainage massage is suitable to reduce swelling;
- a set of exercises to strengthen the muscles in the eye area
It is worth noting that the negative consequences after eyelid blepharoplasty can lead to the patient having to lose the normal rhythm of life for a short period of time for a certain period of time. But the positive result is worth the effort. The rehabilitation period lasts significantly less than the obtained effect.
Eyelid surgery at VIP Academy is safe
Our medical center employs plastic surgeons and ophthalmological surgeons who have already performed more than 5,000 blepharoplasties. take into account the physiology of the entire appendage apparatus of the eyes: muscles, skin and cartilage tissue of the eyelid, subcutaneous tissue and conjunctiva. The doctor accurately determines the amount of intervention in order to achieve a good result and not disrupt the function of the visual organ.
We have a license from Roszdravnadzor to provide plastic surgery services.
Make an appointment with a surgeon by phone or through the website. The manager will answer additional questions via online chat.
TECHNIQUE FOR TRANSCONJECTIVAL BLEPHAROPLASTY
The plastic surgeon performs preoperative markings for transconjunctival blepharoplasty directly on the operating table. The incision site is usually located in the middle of the inner surface (conjunctiva) of the lower eyelid.
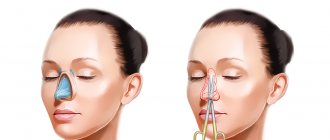
Figure 1. Preoperative view. The changes in the lower eyelid are schematically shown: bags and bruises under the eyes, without pronounced excess skin.
Figure 2. The dotted line shows preoperative markings.
Before eyelid lifting, infiltration is performed - the introduction into the tissue of the lower eyelid to facilitate detachment of a special solution, which consists of a physiological solution with the addition of an anesthetic (pain relief) and adrenaline (for vasospasm and reduction of bleeding). An incision 1.5 - 2 cm long is always made with a scalpel to minimize tissue trauma. There are three packages of hernias on the lower eyelid, which are sequentially isolated and excised.
Figure 3. Making an incision with a scalpel along the preoperative marking line.
Figure 4. Isolation of three hernial bags of the lower eyelid and their removal.
Figure 5. Applying a cosmetic suture to a postoperative wound.
Figure 6. View after transconjunctival blepharoplasty.
A wrapping or subconjunctival suture is applied to the postoperative wound using a self-absorbing thread. Some plastic surgeons do not close the postoperative wound at all when performing transconjunctival blepharoplasty.
The great advantage of this operation is the ease of execution and the absence of postoperative scars.