Excess weight is one of the most pressing problems of our time. According to WHO, over the past 40 years the number of people suffering from obesity has quadrupled. Today their number is 650 million people worldwide. The main cause of the disease is considered to be excess food consumption with insufficient physical activity. The body receives an amount of nutrients that it does not have time to process. Excess is stored in the form of subcutaneous fat.
It should be noted that food is psychologically addictive. At a certain stage, a person who does not have sufficient willpower can no longer stop and continues to consume excessive amounts of food. His weight increases, sometimes reaching enormous levels. To reduce the need for food and achieve weight loss, not only therapeutic but also surgical methods are used. One of the common methods of weight correction is mini-gastric bypass surgery.
Mini-bypass surgery is an operation that can not only reduce the volume of the stomach, but also slightly change the path of food in the digestive tract. Thanks to this, satiety occurs faster during meals, and the amount of nutrients entering the blood decreases. In Moscow, similar interventions are performed by doctors at the Moscow Bariatric Group bariatric surgery clinic. The center is one of the first medical organizations in the Russian Federation that began to carry out such procedures and achieved success in this area.
What is the difference between classic gastric bypass and mini gastric bypass?
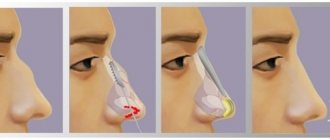
The main difference between mini-gastrobypass and the classic version of the operation according to the method of the German scientist Wilhelm Roux is the number of anastomoses - artificial connections between parts of the intestine. With classic gastric bypass surgery, the surgeon cuts off a small part of the stomach and creates a small ventricle with a volume of about 20-40 ml. The small intestine is divided approximately down the middle. Its lower part is sutured to the newly created ventricle, and the upper part, connected to the remaining lobe of the large stomach, is implanted into the lower gastrointestinal tract. Thus, the doctor makes two anastomoses, one of which is located on the small stomach, the second on the final part of the jejunum.
The mini-gastrobypass technique is generally similar to the procedure described above. However, the small ventricle has an elongated shape and is directly sutured at the level of 150-200 cm from the beginning of the jejunum. Its complete intersection is not performed. Anastomosis is present only at the junction of the ventricle with the middle part of the small intestine. This approach allows Moscow Bariatric Group surgeons to significantly reduce the time of surgery and anesthesia.
Mini-gastrobypass compared to conventional gastric bypass is preferable in the following cases:
- poor tolerance to general anesthesia, need to reduce the duration of anesthesia;
- diseases of the cardiovascular system;
- high risk of postoperative complications;
- insufficient ability to recover in patients with diabetes (fewer number of anastomoses - it is easier for the body to heal damage).
The decision about the optimal method of operation remains with the surgeon. Our doctors accept it based on the results of a comprehensive examination and consultations with related specialists (endocrinologist, gastroenterologist, cardiologist), who will observe you free of charge throughout the course of treatment at the Moscow Bariatric Group.
Preparing for surgery
You can complete all the necessary preparatory activities at our clinic. You do not need to waste time and effort visiting third-party medical organizations. Preparation includes the following types of examinations:
- ECG - allows you to assess the condition of the heart;
- FGDS - used to examine the esophagus, stomach and duodenum;
- Ultrasound of the abdomen - required to assess the condition of internal organs and plan the course of the operation;
- Chest X-ray - allows you to exclude severe pathology of the respiratory system;
- laboratory tests (general and biochemical blood tests, coagulogram, blood group, acid-base balance and electrolytes, test for blood-contact infections) - with their help, the doctor assesses the general condition of the body, predicts possible complications and determines contraindications to surgery, if any.
The examination plan necessarily includes a consultation with a therapist, endocrinologist, and gynecologist (for women). Immediately before the operation, the anesthesiologist who will administer anesthesia will meet with you. Tell your doctors about any health problems you have and provide medical documentation, if available. This will make the operation safer and achieve an optimal result of the procedure.
How is the operation performed?
Our center practices laparoscopic interventions, which means that there will be no unaesthetic scars left on your body. The surgeon, using special instruments, works through 3-4 punctures on the anterior abdominal wall. The length of each of them does not exceed 1 centimeter. Subsequently, neat stitches are placed on the punctures, so that after healing, small, barely noticeable scars remain on the skin.
The operation is performed under general anesthesia. We use anesthetics that ensure easy awakening and the absence of post-anesthesia psychosis. The duration of the procedure is on average 1.5-2.5 hours. During this time you will sleep and wake up in the recovery room. There will be no pain. During the intervention, your condition is monitored by modern expert equipment and an experienced anesthesiologist, so you do not have to worry about your own safety.
Surgical intervention ↑
Gastric bypass surgery is performed using general anesthesia. The surgery lasts from 2 to 4 hours.
Small punctures are made in the abdominal wall, through which a laparoscope is inserted, which is equipped with a miniature video camera and special manipulators. The entire operation is carried out under the supervision of the operating surgeon.
First, the laparoscope is brought to the stomach and small intestine, then the necessary manipulations are performed: a “small” stomach and anastomoses between the stomach and small intestine are created, finally the holes are sutured and a sterile bandage is applied to the puncture sites.
After the operation, the patient requires intensive care and medical supervision; if the patient is feeling satisfactory, the doctor gives permission to transfer the patient to a regular ward.
What causes weight loss
Weight loss after mini-gastrobypass occurs due to two mechanisms. First, due to the reduced stomach capacity, you feel full faster and eat less food. Secondly, due to the fact that food enters the small intestine much lower than it occurs under normal conditions, it does not have time to be completely processed. Accordingly, the amount of nutrients absorbed into the blood is insufficient to maintain the same body weight. Weight begins to quickly decrease as the body compensates for its energy needs by breaking down subcutaneous fat.
Gastric banding
Gastric banding (Bariatric) is a modern, highly effective method of surgical treatment of obesity. During this procedure, a gastric band is placed on the top of the stomach, just below the esophagus. The applied ring gives the stomach an hourglass shape, thereby reducing the volume of the stomach and, accordingly, the amount of food consumed. The food eaten immediately fills the small ventricle and causes a very quick feeling of fullness. Thus, a person can eat very little food at a time, the total number of calories consumed is sharply reduced, and weight loss begins. After surgery, the doctor can adjust the width of the opening for food to pass through and the speed at which it passes through the digestive system. It is also important that the operation can be reversible. Removal of the bandage (if necessary) is also carried out laparoscopically.
Most people go home the same day of surgery. Most people can start working within a week.
The average weight loss is about one-third to one-half of excess weight. This may be sufficient for many patients. Weight loss typically occurs more slowly than with gastric bypass surgery. You should wait until 3 years to lose weight.
Research to date shows that the functioning of the gastrointestinal tract normalizes over time. Even in old age, significant weight loss and improved quality of life have been reported due to this procedure.
These complications or side effects of gastric band surgery may occur:
— The gastric band (ring) may slip partially or completely. — A gastric band (ring) can tear or damage the wall of the stomach. - Heartburn or reflux symptoms may occur. — Bandage tubes may break or leak. The solution to this problem will require minor surgery.
How will you lose weight after mini-gastric bypass surgery?
The effectiveness of mini-gastrobypass surgery is comparable to the classic version of the operation. After it, you can lose about 60-70% of your original body weight. This result is achieved 1.5-2 years after the intervention, subject to all doctor’s recommendations. In the first months, weight loss will be very intense, but later the process will slow down.
On average, our patients lose about 1 kilogram per week. This pace allows you to gradually get rid of obesity, while avoiding the complications associated with too rapid weight loss. The first results of treatment become noticeable by the end of the first month. Throughout the entire period required to normalize your body weight, Moscow Bariatric Group specialists will monitor you and monitor the weight loss process.
How much weight can you lose?
Numerous advertisements give amazing examples of weight loss, however, unfortunately, without surgery you can actually lose only 10% of your original weight.
That is, if your weight was 95 kg, then as a result of a grueling diet, taking medications and biological supplements, you can actually reach 86 kg. Does this suit you? Of course not. That is why the technique of inserting an intragastric balloon appeared. When using this technique, you can lose weight by 20-25% of your initial weight (that is, in our example, you can lose weight up to 70-75 kg). For most people, this kind of “weight loss” is enough for a further comfortable life. However, this applies to people who are slightly overweight. What to do if a person weighs more than 100 (let’s take two examples - 110 and 160) kg, but wants to reduce the weight to 65-70? In this case, the main method of losing weight will be surgery. Of course, weight separately from height and age cannot give an accurate picture, however, most likely, at a weight of 110, banding is indicated (weight reduction to 40% of the original), and at a weight of 160, gastric bypass (weight reduction to 60% of the original). As you can see, the desire to lose weight has stimulated not only manufacturers of nutrition and dietary supplements, but also surgeons in their desire to help you. Today it has been established that you can lose weight from any weight and to any weight, you just need to know when to stop and turn to specialists.
Indications and contraindications for mini-bypass surgery
Indications for mini-gastrobypass surgery do not differ from those for classical Roux-en-Y surgery. The intervention is carried out in the following cases:
- body mass index above 45-50 kg/m2;
- BMI is above 40 kg/m2 if the patient refuses to follow the recommended diet and rapid weight gain;
- the presence of diseases, successful treatment of which is possible only after losing weight;
- diabetes mellitus of non-insulin-dependent type due to obesity;
- lack of effect from other weight loss methods.
The choice in favor of mini-bypass surgery is made when there is a high risk of complications, the need to reduce the time spent under anesthesia or to facilitate the regeneration process as much as possible. To determine the presence of indications, choose the optimal method of work and eliminate contraindications, the clinic’s doctors will provide you with a full range of preoperative diagnostics.
After the examination, our doctor may refuse to perform surgery on you if it would jeopardize your life and health. Thus, mini-gastrobypass surgery is not performed for patients with exacerbation of cardiovascular diseases, blood clotting disorders, or acute infectious diseases. In addition, intervention is contraindicated if the patient is under 16-18 years of age, has acute mental disorders, drug addiction, or alcoholism. The procedure is not indicated for people with a BMI less than 40 kg/m2 and is rarely used as a first treatment option. First, the patient is recommended to try conservative methods of weight correction.
Advantages and disadvantages of mini-bypass surgery
The advantages of mini-gastrobypass surgery include:
- weight loss that is many times greater than that achieved with other treatment methods;
- reducing the risk of heart attacks, strokes and other diseases associated with excess weight;
- complete cure of type II diabetes mellitus in 98% of cases;
- less surgical trauma compared to classic bypass surgery;
- shorter and easier recovery period;
- significant reduction in operational risks;
- reversibility of changes - if necessary, the intestines can be returned to their previous state.
The main disadvantage of the procedure is insufficient absorption of vitamins. They must be taken in tablet form. In addition, dumping syndrome may occur when eating foods rich in simple carbohydrates and fats. In most cases, it manifests itself with vomiting, diarrhea, dizziness and a feeling of heat in the upper half of the body. It should be noted that this is only conditionally a disadvantage. In fact, this reaction to energy-dense foods will keep you from eating them and will provide additional protection against weight gain again in the future.
What recommendations should be followed after surgery?
The recovery period after mini-gastrobypass surgery takes on average 1.5-2 weeks. In this case, discharge from the hospital becomes possible within 5-7 days. Until the sutures are completely healed, it is necessary to avoid significant physical activity, however, walking and exercise therapy with the permission of a doctor are mandatory. Later, you will need to maintain some activity, such as walking or swimming. This will increase calorie consumption and ensure that their intake into the body is lower than energy expenditure.
Correction of the diet is of great importance. It is important that immediately after surgery the diet is liquid and gentle. It is possible to use protein concentrates or broths. After a few days, you will be allowed to eat rougher foods, but the amount of foods with excessively high energy value will need to be significantly reduced. Food intake should be in small portions, 5-6 times a day.
A nutritionist at the Moscow Bariatric Group clinic will develop a diet for you that will meet your needs. Our specialists select the diet in such a way as to provide the patient with adequate nutrition, but to avoid the intake of “harmful” calories. In addition, you will need to take dietary supplements containing calcium, iron and vitamins.
What complications exist and how to deal with them
Like any other operation, mini-gastrobypass surgery may be accompanied by certain complications. During the intervention and in the early postoperative period, you will be under constant medical supervision. They have many years of experience and know how to deal with any undesirable consequences of the procedure. There is no need for you to worry about your safety, our specialists will do this. Later, especially after discharge from the hospital, you may experience the following reactions:
- Dumping syndrome. Occurs immediately after eating or shortly after eating. As a rule, it is associated with errors in diet. Manifested by general weakness, dizziness, feeling of heat. It is easily eliminated by following a diet and goes away within the first year after surgery.
- Deficiency of protein and microelements. You may experience dry skin, weakness, and hair loss. It is necessary to review the diet and add to it foods rich in protein and other substances for life.
- Insufficient weight loss. It is extremely rare. Requires additional examination, lifestyle and nutrition adjustments.
We are ready to support you if any post-operative problems arise. So that you always know who to turn to for help, the Moscow Bariatric Group bariatric surgery center will assign you a personal curator who will listen to you, determine further tactics of action and make an appointment with the necessary specialists. Most often, our patients need additional consultation with a nutritionist, since the vast majority of their problems can be solved by revising their diet and eating regimen.
Vertical gastroplasty
The group of restrictive surgeries combines several operations, the most common of which are vertical gastroplasty, non-adjustable gastric banding and adjustable gastric banding.
Despite the difference in the technical performance of the above operations, they are based on the same principle, which is to reduce the volume of the functioning stomach with the formation of a “small ventricle”. The operating principle underlying the creation of a “small ventricle” is quite simple.
In the intermuscular and submucosal layers of the stomach wall there are nerve endings - baroreceptors (pressure receptors). When interacting with food, baroreceptors send a signal to the hypothalamus, and from there to the cerebral hemispheres of the cerebral cortex, the hunger-satiety center, creating a feeling of satiety in the patient. The formed “pseudopylorus” or bandage promotes the presence of food in the “small ventricle” for a sufficiently long time, increasing the time of exposure of the food bolus to the baroreceptors and prolonging the feeling of satiety when eating a small amount of food. Since these treatment methods are surgical, the indications for their implementation are more stringent than for conservative treatment or installation of an intragastric balloon.
Indications for performing restrictive operations:
- II degree of obesity (BMI from 35 kg/m2 to 40 kg/m2) in the presence of concomitant diseases and the ineffectiveness of non-operative treatment methods;
- III degree of obesity (BMI > 40 kg/m2);
- Young patients (up to 30 years), whose BMI is more than 30 kg/m2, with rapidly progressing obesity, who are unable to strictly follow the doctor’s recommendations when using non-operative treatment methods (for example, installation of an intragastric balloon).
The choice of one or another surgical treatment method is carried out individually for each patient.
As before any operation, the patient must undergo the necessary examination. In this case, the preoperative examination, in addition to standard tests, additionally includes:
- Endoscopy to exclude acute erosive and ulcerative lesions of the gastric and duodenal mucosa and deformations of their lumen;
- Consultation with a gynecologist, for women with III degree obesity;
- X-ray of the skull (sella turcica), which makes it possible to identify indirect signs of pituitary adenoma;
- Ultrasound or computed tomography of the abdominal organs to identify concomitant pathologies, especially the presence of stones in the lumen of the gallbladder.
If a concomitant pathology is detected (gallbladder stones, uterine fibroids, etc.), its surgical treatment can be performed simultaneously with bariatric surgery.
Contraindications to restrictive surgeries are:
- The presence of acute erosions and ulcers of the stomach and duodenum, specific inflammatory diseases of the gastrointestinal tract;
- Pregnancy or planning pregnancy in the next 1.5 years;
- A history of gastric surgery;
- Addiction to alcohol or drugs;
- Long-term use of high doses of non-steroidal anti-inflammatory drugs;
- Pyloric stenosis, varicose veins of the esophagus;
- Large hiatal hernia;
- Emotional instability or mental retardation;
- The presence of hormonally active tumors of the adrenal glands, ovaries, and pituitary gland.
These contraindications in most cases are relative and should be considered in each case individually.
Behavior in the postoperative period After restrictive operations, the patient is not able to take a large amount of food at the same time, regardless of his desire (the volume of the “small ventricle” is 30 cm3); moreover, when eating even a very small amount of food (2-3 tablespoons), a feeling occurs saturation, lasting 4-6 hours. However, there are still nutritional rules recommended for patients after restrictive surgery. For example, it is advisable to separate liquid and solid food intake with a minimum interval of 30 minutes; meals are taken about 4-5 times a day, with mandatory breakfast, lunch and dinner; sharply limit the intake of liquid high-calorie foods, avoid carbonated drinks, etc. Upon discharge from the hospital, each patient receives detailed nutritional instructions, and, if necessary, consultation and observation by a nutritionist.
Restrictive surgeries are the most physiological of all bariatric surgeries. Since their implementation does not require significant restructuring of the gastrointestinal tract, no pronounced metabolic disorders are observed in the postoperative period, which makes these operations very attractive for specialists and patients.
Vertical gastroplasty Vertical gastroplasty has been actively performed since the 50s of the twentieth century, when it was first performed by the American surgeon EE Masson. For 50 years, this operation has not undergone fundamental changes and is currently widely performed in the treatment of obese patients.
Technique of the operation The basis of this operation is the formation of a “small ventricle”, which is achieved by stitching the anterior and posterior walls of the stomach along the lesser curvature, using a special stapler with the application of several rows of titanium staples. In this section of the stomach, the muscle layer is thickest and less susceptible to stretching. Currently, there are several modifications of this operation, but the basic principles of its implementation described above remain unchanged. In our clinic, vertical gastroplasty is performed both openly (through an incision) and laparoscopically (through punctures ranging in size from 5 mm to 2.0 cm), which makes the cosmetic effect as beneficial as possible.
In the classical method of performing vertical gastroplasty, the anterior and posterior walls of the stomach are first sutured with a circular suture apparatus to create a window with a diameter of about 2.0 cm, and then towards the esophagus and along the edge of the calibration probe, the stomach walls are sutured with a linear suture apparatus with the application of 4 rows of titanium paper clips The size of the “small ventricle” being formed is determined using a calibration probe with a diameter of 10-11 mm, installed along the lesser curvature of the stomach. Thus, after stitching the stomach, the diameter of the “small ventricle” is 10-11 mm, the length is about 7-8 cm. Through the created window around the outlet of the “small ventricle”, a polypropylene mesh 1.5-2.0 cm wide is applied along its outer surface and a circumference of 5.0-6.0 cm or a silicone ring (formation of a pseudopylorus).
The pseudopylorus prevents food from quickly leaving the “small ventricle” and also prevents its strong stretching. The modern version of vertical gastroplasty uses the TA-90BN linear suture device, developed in 1991 by AutoSuture specifically for this operation, which allows vertical gastroplasty to be performed by applying just one 4-row linear suture. Polypropylene mesh is also most often used as a “pseudo-gatekeeper”. The use of the TA90-BN device can significantly reduce trauma to the stomach walls and more clearly calibrate the size of the “small ventricle” being formed. Laparoscopic performance of this operation allows the patient to be discharged from the hospital within 24 hours.
The most common complications and side effects One of the advantages of vertical gastroplasty is the absence of the need for significant anatomical restructuring of the gastrointestinal tract, and as a result, the absence of serious side effects. Some patients have iron deficiency anemia, which is corrected by several courses of iron-containing medications. Among the most common specific complications, the following can be noted: narrowing of the outlet section of the “small ventricle”, atony of its walls, inflammation of the mucous membrane of the esophagus and “small ventricle”, acute dilation of the “small ventricle”. All of the above complications, with the exception of the last one, can be managed conservatively and do not require re-operation. With acute enlargement of the “small ventricle,” surgical treatment may be required in some cases.
Currently, vertical gastroplasty is the most effective of restrictive operations. Our experience in performing this operation (since 1991) allows us to evaluate long-term results showing the stability of the achieved weight for -10 years in the vast majority of patients. Combined operations.
What is the cure for diabetes mellitus?
Cure from non-insulin-dependent diabetes mellitus occurs through two mechanisms. First of all, the concentration of fatty acids decreases in the body of a losing weight person. Their negative impact on the receptors responsible for processing sugar is reduced. Glucose begins to be better absorbed and its content in the blood returns to normal.
The essence of the second mechanism is as follows. In the human duodenum, anti-incretins are formed - substances that impair the absorption of carbohydrates. Since after mini-gastrobypass surgery food from the stomach goes directly into the jejunum, anti-incretins are no longer created in the same amount. This promotes better processing of sugars and their absorption by the body's cells.
Side effects
There are also some side effects after bariatric surgery:
- May contribute to mineral and vitamin deficiencies.
- Lifelong vitamin and mineral supplements may be required.
- You may feel nauseous.
- Leads to low blood sugar.
- They can cause inflammation, ulcers and hernias.
- It is necessary to see a doctor.
- A strict and specific post-operative diet must be followed.
- Repeat surgery may be required.
Surgery is the best choice for those who are overweight and/or have life-threatening underlying medical conditions. Before deciding on anything, consult your doctor, form your opinion about such operations and the clinic to which you will entrust this procedure. Remember that these surgeries are NOT FOR THOSE who can lose weight by exercising and eating right.