Content
- Types of surgical treatment for bunions
- Common techniques
- How is a bunion removed?
- Contraindications
- Preparing for surgery
- Approximate cost of the operation
- Rehabilitation
Conservative treatment of this common pathology is effective only at the initial stage of the disease, when the thumb deviates slightly (up to 15 degrees) outward, there is no pain yet, and the lump itself looks like a small tubercle.
If a bunion appears on the leg, timely contact with an orthopedist allows you to correct the deformity using conservative methods
Unfortunately, not all people pay attention to changes in the foot before pain symptoms appear, and the doctor examining the patient is forced to state that the situation is advanced and only removal of the bone on the big toe can correct the pathology (the operation allows not only to get rid of pain and prevent the progression of the disease, but also to restore the arch of the foot).
Indications for surgical treatment
Again, the indications depend on the disease:
- For hallux valgus, the main indication is the adult age of the patient. Because conservative treatment will only save in childhood, or in the initial stage of the disease
- In case of congenital clubfoot, the indications include a severe degree of the disease. And the disease itself can only be treated surgically. That is, the disease itself is an indication.
So, each foot disease has its own indications. Mostly, surgical intervention is resorted to if conservative treatment does not help.
Types of surgical treatment for bunions
The operation to remove a bunion is carried out after additional diagnostics, which allows you to accurately assess the degree of deformation and identify concomitant pathologies and diseases. The choice of surgical technique (there are about 100 different methods) is influenced by:
- type of deformation;
- the condition of the bones and soft tissues of a particular patient;
- presence of somatic diseases.
Since low-traumatic methods and modern anesthetics are currently used in most cases to remove bunions, the age of the patient does not affect the choice of surgical procedure.
Possible application:
- Osteotomy, which is used in most cases as the most effective method. With any type of osteotomy, during surgery, the tissue is cut over the deformed joint, the bone is intersected (transversely closer to the nail or at its other end, Z-shaped or along the main phalanx), bone fragments are installed in the correct position and fixed with staples or a special screw.
- Arthrodesis. This type of surgery is performed in very rare cases, since the main purpose of the operation is to create a fixed joint that does not allow the foot to be completely restored. The indication for this type of operation is a severely damaged thumb joint, which cannot be returned to the correct position using osteotomy. During the operation, the metatarsophalangeal joint is removed, and the bones are connected to each other. The disadvantage of this method is the pain at the fusion site that occurs after exercise, as well as the need to constantly wear orthopedic shoes.
- Resection arthroplasty, in which part of the articular surface is removed. In this case, a cavity remains between the parts of the bone, which is filled with connective tissue during the healing process (thus forming a false joint). This operation does not provide complete restoration of foot function.
- Correction of the transverse arch of the foot. With this type of surgery, it is not the joint and bone that are corrected, but the soft tissue around the problem area. During the operation, the tendons of the adductor hallucis muscle are transplanted from the big toe to the 1st metatarsal bone, the muscle no longer holds the big toe in a deflected position, the angle between the bones of the foot changes, and the arch of the foot restores its normal shape. The method is effective in the early stages of the disease.
- Exostectomy, in which the cone itself (part of the head of the metatarsal bone) is excised, as well as the soft tissue located around the affected joint. The gait after the operation is restored, the pain is eliminated, but relapses are possible.
Symptoms of the disease
This disease develops rather slowly and is therefore difficult to notice. At first, it seems to a person that the usual shoes have become uncomfortable.
After this, pain occurs in the feet.
gradually appears - deviation of the thumb and the formation of a so-called bone near its base. At the same time, the remaining fingers take the shape of hammers. A person may suffer from fatigue or have difficulty choosing shoes. He may also develop calluses that make walking difficult.
The main manifestations of hallux valgus are as follows:
- a soft formation appears, which is accompanied by the fact that the skin in the joint area turns red, pain appears as the joint capsule becomes inflamed;
- the thumb changes its shape, becoming crooked;
- a hard lump forms in the area of the first phalanx;
- callus develops and the skin becomes irritated;
- pain appears while walking;
- the thumb loses its mobility. Over time, other fingers may lose motor activity.
There is a simple classification, according to which there are several stages of development of hallux valgus:
- 1st degree. The toe moves less than 20 degrees. In this case, there is no discomfort.
- 2nd degree. The joint moves 20-30 degrees. In this situation, a person feels minor pain.
- 3rd degree. There is a displacement of the joint by 30-50 degrees. In this case, there is constant pain in the area of the big toe. These sensations prevent a person from performing his usual actions in full.
- 4th degree. The joint moves more than 50 degrees. This condition is characterized by severe pain, discomfort when walking, difficulty choosing shoes, and the formation of calluses.
Common techniques
Surgery on the bunion of the big toe with the intersection of the bone is most often performed using the method:
- Scarf osteotomy. Used for moderately severe hallux valgus deformity. Allows you to shift in the longitudinal direction and rotate part of the head of the metatarsal bone, lengthen or shorten the first metatarsal bone, shift bone fragments, which allows you to achieve greater proportionality of the joint and reduce the load on the joint and the inside of the foot. The technique gives good results in combination with soft tissue correction.
- Austin/Chevron osteotomy, in which a V-shaped transection of the first metatarsal is performed. Used in cases of minor valgus deformity, it allows the head of the metatarsal bone to be displaced by 1/2 of its width (if the displacement is more than 1/2 of the width of the bone, the stability necessary for bone fusion may not be enough).
- Akin osteotomy, which is performed on the main phalanx (at the level of the proximal part of the tubular bone adjacent to the epiphyseal plate). Accompanied by mandatory manual correction of hallux valgus. The bone is divided parallel to the metatarsophalangeal joint and the nail bed of the big toe, and the wedge-shaped fragment is removed.
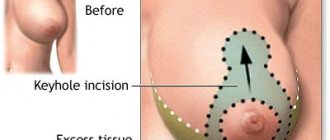
Various methods of cutting the bone when removing a bunion.
Surgery to remove a bunion on the big toe can also be performed:
- According to the Weil method (oblique osteotomy of the small metatarsal bones). Allows you to move the bones towards the center and in the longitudinal direction, returns the head of the metatarsal bone to its normal position and helps eliminate hammertoe deformity.
- According to the Schede-Brandes method (marginal resection of the medial bone outgrowth (exostosis)). During the operation, the bone on the lateral surface of the 1st metatarsal bone and the proximal part of the main phalanx of the big toe are removed, a plaster splint is applied to fix the foot in a certain position, and then traction is performed on the nail phalanx of the big toe for 2 weeks.
A good cosmetic result is obtained by surgery to remove bunions using the Wreden-Mayo method (consists in removing the head of the 1st metatarsal bone along with the bump), however, due to the elimination of the main supporting platform of the foot when walking, a violation of the supporting function of the foot is observed after the operation.
Removal of the bunion on the big toe using the Chalkin method (intersection of the bone with rotation of the head of the 1st metatarsal bone) and trapezoidal wedge resection of the 1st metatarsal bone using the Bohm and Reverden method do not eliminate the medial deviation of the 1st metatarsal bone and do not restore the arch of the foot, therefore, they are often accompanied by relapses.
The patient may be offered reconstructive surgery aimed at correcting several components of the foot deformity:
- The method of Kramarenko and Boyarskaya, during which, after surgery using the Schede-Brandes method, to eliminate the medial deviation of the 1st metatarsal bone, a transverse osteotomy is performed distal to the metatarsocuneiform joint, and a graft formed from previously removed parts of the bone is hammered into the resulting wedge-shaped gap. A transverse ligament of the foot is formed from Mylar tape, which holds the 1st metatarsal bone in the correct position (the tape is sutured to the edges of the capsules of the 1st and 5th metatarsophalangeal joints). After surgery, a plaster cast is applied to the foot for 4-5 weeks.
- Operation Korzh and Eremenko, in which the bone does not intersect, since the defect is eliminated by removing the 1st metatarsocuneiform joint. The transverse ligament of the foot is formed from the tendon of the long extensor of the 4th toe.
- An operation using the CITO method, which is accompanied by the formation of a transverse ligament of the foot from a Mylar tape in the form of a figure eight according to Klimov.
Performing an operation using traditional surgical methods.
If necessary, endoprosthetics is performed, in which the deformed joint is completely removed and replaced with an artificial one.
The best clinics for foot surgery
Regardless of the cause of leg pain, qualified, effective assistance will be provided in the following clinics:
- MEMORIAL – Türkiye, Istanbul;
- CHARITE – Germany, Berlin;
- MEDICANA – Türkiye, Istanbul;
- ASSUTA EXPRESS MEDICAL – Israel, Tel Aviv.
Rating of countries where foot surgeries are performed
Successful low-traumatic foot surgery is a reality in the following countries:
- Switzerland, Germany;
- Israel, Finland;
- Türkiye, South Korea.
The level of domestic medicine does not yet allow us to give highly favorable prognoses.
How is a bunion removed?
Previously, surgery to remove a bunion on the big toe was quite traumatic (the bunion was removed, the joint was secured with staples and pins), so complications often arose, and the rehabilitation period was long. Due to the imperfection of previously used techniques, reviews of the operation to remove bunions were rather negative, since the high level of trauma accompanying the surgical intervention caused pain in patients for a long period, and relapses were often observed.
Currently, bunions can be removed with minimal trauma using:
- Minimally invasive techniques in which the incision does not exceed 3 mm (with significant deformation - 10 mm). Surgical manipulations (intersection of the bone and displacement of its parts) are carried out through this small incision under X-ray control. The advantages of minimally invasive osteotomy include a short rehabilitation period and almost invisible scars, pain and the risk of complications are minimal. Minimally invasive operations do not require general anesthesia (local or epidural is used), but can only be used for mild deformities of the thumb.
- A laser that allows you to remove bone tissue in the thinnest layers, thus maintaining joint mobility. The rehabilitation period is shorter than when using a traditional surgical kit (drill, knitting needle, screwdriver, clamp). Laser removal of bunions is used if the patient does not have other foot deformities or complications of hallux valgus.
Minimally invasive and traditional methods that are used for various types of hallux valgus.
Access during the operation can be:
- open (the tissue is cut to the bone using a scalpel, the surgeon, thanks to a visual review, controls the correction process);
- closed (manipulation is carried out through a small incision, control is carried out using x-rays).
Laser bunion removal involves grinding down the bunion on the foot until it is completely aligned with the lateral surface of the foot, which is carried out through a small incision. To remove a bone using a laser, resurfacing is accompanied by:
- exostectomy;
- osteotomy;
- resection arthroplasty.
The advantages of laser removal of hallux valgus include:
- disinfection of the wound under the influence of a laser, which minimizes the risk of infection;
- minimal blood loss due to the small size of the incision through which manipulations are performed;
- no effect on surrounding tissues;
- fast recovery;
- shorter operation time (takes 1 hour, while removal of a lump using traditional surgical methods takes about 2 hours);
- no need to wear a cast after surgery.
The most minimally traumatic and effective method is to remove a bone on the thumb using a laser.
Removing a bunion using any method consists of several stages. Most often during the operation:
- An incision is made on the inside of the big toe phalanx.
- A capsulotomy is performed (dissection of the capsule of the first metatarsophalangeal joint).
- Excision of the bone outgrowth (bump removal) is performed.
- The first bone of the metatarsus is sawed (an osteotomy is performed).
- The surgeon moves fragments of the metatarsal bone, changing the axis of the deformed area.
- The bone is fixed with titanium screws or staples.
- The capsule and incision are sutured.
- A sterile bandage is applied to the access site.
- A fixing bandage or plaster is applied to the foot (depending on the type of operation).
Titanium screws are not removed if there is no discomfort.
Foot diseases
There is a special science that studies foot diseases. It's called podiatry. There are many types of foot diseases. Some diseases can be cured at home, while others require mandatory treatment by a specialist. They can also be either congenital or acquired.
Below is a list of the most common foot diseases:
- Hallux valgus deformity of the big toe. The disease is characterized by a protruding bone. The bunion protrudes as a result of the deviation of the big toe into the foot. With this disease, it is not recommended to wear tight shoes. It will cause pain and discomfort. Pain may also occur if the patient is diagnosed with arthritis. Treatment is carried out with painkillers; there are cases when surgery is required.
- Calluses and corns. They are hard, rough patches of skin. This rough skin has a protective function. They occur as a result of wearing tight shoes for a long time. When the shoes are removed, the pain subsides. A patch will help in the fight against this disease.
- Gout. This is a type of arthritis. There is severe pain, redness, and swelling. Occurs as a result of increased levels of urea in the blood. The inflammatory process can last for 7 days. Anti-inflammatory drugs will help.
- Plantar warts. This disease has a viral etiology. The virus enters through cracks in the foot. Salicylic acid is used for treatment. If the case is severe, they resort to surgery.
- Athlete's foot. This disease is caused by a fungus. The disease is transmitted by contact with the fungus itself, that is, by wearing someone else's shoes, or while in the pool and gym. It develops very rapidly and remains in the shoes themselves. Antifungal agents are used in treatment.
- Nail fungus. This disease is transmitted through contact with an infected person. Penetration occurs through microcracks in the nail. The disease does not cure itself. For treatment it is necessary to resort to antifungal drugs.
- Flat feet. The disease is characterized by changes in the foot. The disease can be inherited or develop as a result of injury. It can also occur due to certain diseases, such as arthritis. Pain occurs when standing for a long time. Difficulties arise in choosing shoes. For treatment, special physical therapy is used, as well as specialized shoes.
- Diabetic foot. Deformation of the foot with the formation of ulcers and pustules on it. The disease occurs due to excess sugar in the blood. For treatment, you must first normalize your sugar and then use antibiotics.
- Congenital clubfoot. The disease occurs in children. This is a change in the foot in which the sole and the foot itself point inward. For treatment, plaster casts, bandages, surgery, physiotherapy, massage and more are used.
- Varus deformity of the foot. The disease occurs in both adults and children. Characterized by curvature of the arches and axis of the foot. The disease is similar to clubfoot. The treatment is very long and difficult. Therapeutic gymnastics, physiotherapy, the use of specialized insoles, massage, and surgical treatment are carried out.
- Mortan's neuroma. The disease is characterized by thickening of the plantar nerve of the foot. There is pain between the fingers. Specifically, between the third and fourth. Treatment includes physiotherapy, changing shoes and more.
Contraindications
Although leg surgery to remove a bone is usually performed using low-traumatic techniques, there are a number of contraindications to its implementation. The operation is contraindicated for:
- thrombosis, which is accompanied by inflammation of the veins and bleeding disorders;
- diabetes mellitus, obesity;
- cardiovascular failure;
- poor circulation of foot tissues;
- pathologies of the musculoskeletal system.
Removing a bunion with a laser has virtually no contraindications, but a preoperative examination is necessary before the procedure.
Contraindications to surgical treatment of the feet
Main contraindications include:
- Severe peripheral vascular disease.
- Destruction of the peripheral nervous system as a result of diabetes mellitus.
- Diseases of the hematopoietic organs.
- Infections with the formation of pus.
If any of the above points are present, surgical intervention is not permissible. In this regard, before any treatment it is necessary to consult a specialist. Only a specialist can explain and prescribe a favorable treatment method.
Preparing for surgery
Before removing bunions, it is necessary to undergo a thorough diagnosis to identify all pathologies of the foot - x-rays of the foot from different sides or magnetic resonance imaging.
In addition to removing the big toe bunion, surgery may include eliminating hammertoes in other toes, etc.
As part of the preoperative examination, the patient is sent for tests:
- blood (general, biochemical, sugar, clotting);
- urine (general analysis);
- to detect hepatitis and HIV;
- ECG;
- fluorography.
Alternative Treatments
Often people who are faced with such a problem ask themselves first of all the question: how to remove a bunion using folk remedies? It should immediately be noted that using alternative medicine it is impossible to completely correct this kind of deformation. Bunions on the feet cannot be removed using folk remedies, but such recipes significantly help relieve pain and eliminate redness.
For this purpose, various means are used, and the most popular can rightly be called iodine. It is used in conjunction with other excipients. For example, you can use grated soap, which is used to massage the skin in the “bones” area, and then thoroughly rinse off its remnants with water. Afterwards, a mesh is drawn on these places with iodine. In addition, “bumps” on the legs can be smeared with camphor oil and then with iodine. Before such a procedure, it is advisable to steam your feet and dry them with a towel.
Propolis can be used with the same success: it is heated in the hands until soft, and then applied to the protruding “bones” and the propolis is fixed with a dry bandage. Ordinary potatoes are also an excellent remedy: they are used raw (then a gruel of grated tubers is applied to the “cones”) or a decoction is used. In this case, the pan is filled 2/3 with peelings and filled with water. Next, they are boiled for 15 minutes, after which the broth is poured into a bowl of warm water. Then your feet soak in this bath for about half an hour, and if you carry out this procedure several times a day, then after a couple of weeks the “bones” will stop bothering you.
In addition, you can also use ointment. To prepare it, a fresh egg with a white shell is poured with vinegar and left alone for several weeks. As soon as the egg has dissolved, the remains of its shell are thrown away, and 1 tbsp of melted lard and 10 g of turpentine ointment are added to the egg itself. This ointment is usually applied to the “bones” every other day, alternating with the use of iodine. In addition, you can also use honey heated in a water bath as a rubbed ointment.
During therapy using folk recipes, you can also take internal medications. For example, decoctions and tinctures of medicinal herbs known for their diuretic effect. These can be birch buds, horsetail, lingonberry and bearberry leaves. However, no matter which prescription a person prefers, it must be previously agreed with his own doctor.
Approximate cost of the operation
Since free hallux valgus surgeries in public institutions require a referral from an orthopedist and a wait in line for elective surgery, patients are often interested in how much it costs to remove a bunion.
The cost of the operation is influenced by the qualifications of the doctor, the methodology, the status of the clinic (private, municipal), the equipment and drugs used. On average, the price varies from 200 to 1000 dollars (in metropolitan areas the cost of the operation is higher than in the regions).
Since the cost of surgery is influenced by many factors (including payment for anesthesia, etc.), it is necessary to call the clinic to clarify the information. Before removing a bunion on your big toe, you must consult with the surgeon of your chosen clinic about possible options for the operation.
The cost of laser bunion removal is higher than other surgical methods.
Ankle surgery
Ankle joint surgeries are performed to treat arthrosis. This is a dangerous chronic disease that is associated with the gradual destruction of the joint. Methods of conservative treatment of arthrosis will not completely restore the ankle, but will only stop its further development.
In the later stages of arthrosis, if the disease causes pain and prevents the patient from walking, surgery is prescribed. It can be carried out in different ways:
- athrodesis - strengthening the bones of the ankle from the inside, as a result of which they acquire an anatomically correct position, and the patient does not experience pain;
- Ankle replacement surgery is a procedure after which the patient will be able to fully resume physical activity without experiencing pain.
Another case in which only surgery can help is ruptured ligaments and tendons of the ankle joint. Such injuries can be related to sports or happen at home. If some of the fibers remain intact, there is a chance to be completely cured without surgery. In cases where the ligament is completely divided into 2 parts or the tendon is torn from the bone, these tissues must be connected with a suture. An incision or small punctures are made on the skin at the site of the injury, through which the ligament or tendon is restored.
Recovery after surgery
Successful surgery does not guarantee that the patient will fully recover. In the postoperative period, it is necessary to undergo a number of procedures. Their goal is to strengthen the muscles and ligaments of the foot, restore flexibility to the tissues, and normalize blood circulation in the legs.
Within 1-2 months after surgical restoration of the foot, it is recommended to perform the following procedures:
- gymnastics - a set of simple exercises to increase elasticity and strengthen the muscles of the foot;
- massage is a good way to normalize blood circulation in the operated area, improve the supply of tissues with oxygen and nutrients;
- physiotherapy is a set of measures aimed at irritating tissues, improving blood circulation and stimulating regeneration processes.
Foot surgery includes both emergency and elective operations. They are carried out according to the doctor’s decision, including to correct the anatomical position of the foot. During the intervention, it is possible to get rid of chronic pathologies of the foot structure, which are accompanied by pain and progress with age. Drug treatment in such cases is ineffective, and after the operation the patient will be able to walk without pain and complications. Rehabilitation for simple operations takes 1-2 months, but this indicator varies from person to person.
Amputation of fingers
The main indication for amputation of the fingers is considered to be trauma with complete or partial separation. When avulsion occurs, the surgeon is faced with the task of closing the skin defect and preventing scar formation. In the case of severe crushing of soft tissues with their infection, there may be no opportunity to restore adequate blood flow, and then amputation is the only treatment option. It is also carried out in case of necrosis of soft tissues and elements of the finger joints.
If during the injury several fractures occur, bone fragments are displaced, and the result of organ-preserving treatment is a motionless, crooked finger, then surgery is also necessary. In such cases, the absence of a finger causes much less discomfort when using the brush than its presence. This indication does not apply to the thumb.
Another reason for amputation of fingers can be damage to tendons and joints, in which preservation of the finger is fraught with its complete immobility, disrupting the functioning of the remaining fingers and the hand as a whole.
Distribution of finger and hand amputations by prevalence
The choice of amputation height depends on the level of damage. Always take into account the fact that a stationary or deformed stump or a dense scar interfere with hand work much more than the absence of an entire finger or a separate phalanx. When amputating the phalanges of long fingers, an operation that is too gentle is often performed.
When forming a stump, it is important to ensure its mobility and painlessness; the skin at the end of the stump should be mobile and not cause pain, and the stump itself should not be thickened in a flask shape. If it is technically not possible to recreate such a stump, then the level of amputation may be higher than the edge of the finger injury.
When performing operations on the fingers, the location of the lesion, the profession of the patient, and his age are important, so there are a number of nuances that surgeons know and must take into account:
- When amputating a thumb, they try to preserve as long a stump as possible; even short stumps are preserved on the ring and middle fingers to stabilize the entire hand during movements;
- The inability to leave the optimal length of the finger stump requires its complete removal;
- It is important to maintain the integrity of the heads of the metacarpal bones and the skin of the spaces between the fingers;
- They try to keep the little finger and thumb as intact as possible, otherwise the support function of the hand may be impaired;
- The need to amputate several fingers at once requires plastic surgery;
- If the wound is heavily contaminated, there is a risk of infectious lesions and gangrene, plastic and gentle operations can be dangerous, so complete amputation is performed;
- The patient's profession affects the level of amputation (for people with mental work and those who perform delicate work with their hands, it is important to perform plastic surgery and maximum preservation of the length of the fingers; for those who are engaged in physical labor, amputation to the maximum extent can be carried out for speedy rehabilitation);
- The cosmetic result is important for all patients, and in some categories of patients (women, people in public professions) it becomes crucial when planning the type of intervention.
Disarticulation is the removal of fragments or the entire finger at the joint level. For pain relief, an anesthetic is injected into the soft tissues of the corresponding joint or into the area of the base of the finger, then the healthy fingers are bent and protected, and the person being operated on bends as much as possible, and a skin incision is made on the back side above the joint. When removing the nail phalanx, the incision is made 2 mm towards the end of the finger, the middle - 4 mm and the entire finger - 8 mm.
After dissection of the soft tissues, the ligaments of the lateral surfaces are intersected, the scalpel enters the joint, the phalanx, which is to be removed, is brought out into the incision, and the remaining tissues are intersected with a scalpel. The wound after amputation is covered with skin flaps cut from the palmar surface, and the sutures are necessarily placed on the non-working side - the back.
Maximum tissue savings, the formation of a flap from the skin of the palmar surface and the location of the suture on the outside are the basic principles of all methods of amputation of the phalanges of the fingers.
Long toes
Too long toes are a relatively common anatomy and tend to be a cosmetic concern for women more often than men. The most common is the long second toe. The so-called Greek foot type. Girls and women are often embarrassed by such features of their feet. They do not wear open shoes and generally narrow ones, which can lead to the formation of a hammertoe deformity of the 2nd toe and a painful callus in the projection of the proximal interphalangeal joint. Because the second toe suffers from repetitive microtrauma in closed shoes.
Pain often manifests itself in tight, ill-fitting shoes. Painful calluses on the fingers can prevent you from wearing stylish shoes even for a short time (1-2 hours a day).
Of course, other toes may also be too long. For example, abnormally long first, third or fourth toes.
Contacting the doctor
If an ordinary wet callus forms in the area of the little finger, you can treat it yourself. But, if suppuration appears, the patient is advised to consult a doctor.
If the formation is excessively large, the patient should consult a doctor. A person should know that timely seeking help from a specialist will eliminate the development of undesirable effects.
What is forbidden to do
When a wet callus forms, it is necessary to adhere to certain rules in treatment. It is strictly forbidden to pierce a callus at home, as this can lead to the development of an infectious process and the appearance of more serious complications.
If the callus has burst, it is forbidden to remove the skin, as it protects the wound from infection.
Treatment of a burst callus
Quite often it happens that the callus on the little finger bursts on its own. In this case, it is necessary to carry out its treatment. First of all, it is recommended to steam the formation. If dirt has accumulated under the skin, it must be removed.
The formation must be treated with hydrogen peroxide. After this, an ointment is applied to the callus, which has antiseptic and disinfectant properties. In order to eliminate the possibility of infection, a patch or sterile bandage is applied to the callus.