Mechanism of appearance and ICD-10 code for eyelid deformities
The pathology is accompanied by tucking of the skin. There are two deformations: entropion - inversion and ectropion - outward.
Eversion of the lower eyelid - code according to the international classification H02.0 - is more common. The situation is explained by the structure of cartilage. In the lower ones they are smaller. Cartilage is easily subject to pathological changes under the influence of unfavorable factors of the external and internal environment. The deformation leads to a cosmetic defect and the development of secondary complications.
The causes and characteristics of deformations are identified.
Ectropion
Ectropion of the eyelid is a pathological condition of a loose fit of the edge of the eyelid to the eye. An eversion occurs. Main causes:
- Senile form, resulting from involutional changes in the ocular apparatus.
- Pathological changes in tissue - loss of elasticity, skin tone - around the eye lead to the development of the disease.
- Eversion associated with chronic inflammatory eye diseases. Blepharitis and conjunctivitis provoke spasm of the musculus periorbitalis.
- Congenital ectropion is caused by a violation of formation in the embryonic period.
- Volvulus may be one of the manifestations of Down syndrome, Miller syndrome, or lamellar ichthyosis.
- The defect occurs after unsuccessful plastic surgery, which is accompanied by the removal of a skin flap and the placement of a large implant in the cheeks.
- Autoimmune connective tissue diseases: SLE, dermatomyositis, scleroderma.
Ectropion is provoked by injuries, burns, tumors.
Both deformities have similar symptoms:
- Excessive tearing.
- Severe swelling, maceration of the pathological area.
- Unpleasant sensations in the form of a foreign body.
Symptoms and diagnosis
Almost all symptoms observed with entropion are associated with direct contact of the eyelashes and the conjunctiva:
- Itching;
- Foreign body sensation;
- Redness of the mucous membrane;
- Injection of blood vessels (visible inflammation);
- burning or soreness;
- Copious discharge from the eyes of a watery nature (due to two reasons: hyperproduction of tear fluid, trying to “wash away” the foreign body, and disruption of the natural outflow of tears);
- Inability to look at light (photophobia).
- Dryness of the eye (develops due to incomplete closure of the eyes during blinking movements). This symptom may be accompanied by a feeling of sand in the eyes.
All these signs are expressed most clearly when blinking.
Long-term entropion can lead to clouding of the cornea and cause decreased visual acuity. In addition, due to impaired tear outflow, there is a risk of developing infectious and inflammatory diseases of the eye (blepharitis, conjunctivitis, keratitis).
Causes of pathology
Ectropion can develop due to:
- Rarely occurring congenital pathological conditions in which the volume of muscles and the area of the skin of the eyelids is less than necessary for a tight fit of the latter to the eyeball. One example is Down syndrome.
- Paralysis of the facial nerve or cerebrovascular accident with the development of hemiparesis. With these diseases, ectropion of the lower eyelid often develops, since the innervation of the facial muscles is disrupted and, accordingly, their tone decreases.
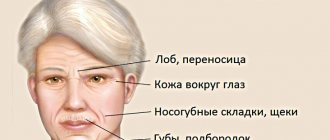
- Age-related changes in the subcutaneous tissue, skin and muscles, as a result of which they lose their tone and elasticity with the simultaneous gradual development of gravitational ptosis of the soft tissues of the face.
- Systemic autoimmune connective tissue diseases (ichthyosis, systemic lupus erythematosus, scleroderma, dermatomyositis, etc.).
- Cicatricial deformation of tissue in the periorbital region and in the eye area. Scars can develop after mechanical trauma or burns.
- Plastic surgery on the face. Due to the frequent plastic surgeries on the face in recent years, eyelid inversion after blepharoplasty has become the most common complication. It can be caused by both cicatricial changes after transconjunctival blepharoplasty and removal (usually by a surgeon with insufficient practical experience) of a piece of skin whose dimensions exceed the possible area of the skin flap in a particular patient, resulting in open areas of the sclera. In addition, ectropion of the eyelids can occur as a result of severe ptosis of the tissues of the buccal areas with depression of the soft tissues of the periorbital area, not only due to their involutive changes, but also as a result of surgery with placement of implants in the buccal areas.
- Inflammatory processes accompanied by increased tone (spasm) of the periorbital muscle (blepharitis, conjunctivitis, dry eye syndrome).
- The presence of a tumor in the orbital or facial area.
Eversion of the upper eyelid, compared to the lower eyelid, is much less common, which is due to some differences in their anatomical structure. The cartilage tissue contained in the eyelids in the form of a plate gives them a certain density and configuration. In the lower ones, the cartilaginous plates are thinner and their density is less than in the upper ones, which provides the latter with a higher degree of resistance to changes in position and deformation. How to correct lower eyelid inversion?
Congenital eversion
An extremely rare pathology explained by the shortened dimensions of the cutaneous-cartilaginous plate of the lower eyelid. Often combined with other autoimmune diseases.
If the deformity is not clearly expressed, the disease does not require treatment. Surgical intervention to narrow the distance to the ciliary edge is carried out only in case of a significant deviation from the norm.
For example, when a child sleeps, a gap is noticeable, during the day the baby is bothered by constant lacrimation, and vision decreases.
Spastic eversion
This form of the disease develops as a result of chronic inflammatory processes occurring in the area of the eyelids and conjunctiva.
Such conditions lead to constant tension in the muscle fibers and spasm of the orbicularis oculi muscle.
Mechanical eversion
Mechanical ectropion is a displacement of the eyelid under the pressure of a volumetric neoplasm formed in the eye area.
Most often, the pathology occurs in elderly patients. Correction of deformity is possible only after removal of the formation.
Paralytic ectropion
Paralytic ectropion is a drooping eyelid due to paralysis of the facial nerve and decreased tone of the facial muscles.
Treatment methods and prognosis will depend on the cause and persistence of the condition. If the condition worsens temporarily, you can get by with the prescription of moisturizing medications to prevent the cornea from drying out.
With complete paralysis of the facial nerve or progression of the disease, surgical intervention is indicated.
Cicatricial eversion
In this case, we are talking about pulling outwards and shortening the eyelid plate as the skin scars at the site of the scar maturation.
Pathology is diagnosed at any age. The main reason is trauma, burns, surgery and some skin diseases.
Treatment is surgery to excise the scar followed by correction of the eyelid position. If the deformity is severe, skin grafting may be required.
Surgery to remove eyelid inversion
There are two ways to eliminate the complication: surgical and conservative. The first option involves the use of gymnastics and massage, which stimulate the growth of the tone of the circular muscle. Surgical methods are prescribed depending on the patient’s age, type of defect, and condition of facial tissues. The doctor needs to know the following information:
- the presence of scars or other damage to the skin;
- the cause of ectropion;
- condition of soft tissues in the eye area;
- How weakened are the ligaments that hold the corners of the eye in the desired state?
The task of surgery is to transport the musculoskeletal structure of the eyelid to the desired position and fix it there. This procedure can only be performed by a qualified plastic surgeon or ophthalmologist in a special department. The initial stage of the manipulation is a meeting with the surgeon, who prescribes the necessary tests for the patient. Among them:
- fluorography;
- general blood and urine analysis;
- blood biochemistry;
- electrocardiogram;
- blood for platelets
If there are pathologies, or depending on the general condition and age, the doctor may prescribe additional tests or a consultation with a related specialist.
The duration of the operation is 1-3 hours, depending on the degree of complexity and the chosen method.
In addition to eliminating ectropion and normalizing the natural process of tear secretion, you can get rid of hernial protrusion in the eyelid area, lift the upper corners of the eyes, and remove excess skin. All these nuances of the operation should be discussed during a consultation with a doctor.
Incisions during surgery, as with blepharoplasty, will be made in the natural folds of the eyelids and stitched together in a special cosmetic way, which will help avoid the formation of scars.
Immediately after the operation, the patient will need to stay in a hospital for 24 hours, under the supervision of a doctor. And after discharge, it is worth visiting a doctor for a consultation, only he will be able to control the correct tightening of the tissues and evaluate the result of the correction. For two weeks after the procedure, swelling may remain on the face. They will be most pronounced in the first few hours after the manipulation.
To alleviate the condition, the doctor may prescribe cold compresses and physical procedures. This will speed up the process of resorption of swelling and tissue regeneration.
Classification
The classification of forms of entropion of the upper and lower eyelids is determined by the causes of the disease. There are two types of entropion - congenital and acquired.
- Congenital is diagnosed from childhood, it manifests itself if there is a genetic tendency;
- Acquired volvulus can occur for a number of reasons. These are injuries, tumors, weakening of the eyelid muscles, and a number of diseases of vital systems.
There are 4 types of acquired entropion:
- Mechanical - appears as a tumor complication. New growths cause tissue to grow and distort the eyelids. When treating mechanical entropion, the main goal is tumor removal. Then you can correct the shape of the eyelid, and it will take an anatomically natural position.
- Cicatricial - with this form of the disease there is a scar that appears between the eyelids and the mucous membrane of the eye (conjunctiva). The cause of cicatricial volvulus is trauma, burns (including chemical ones), and severe inflammation. The condition gets worse quickly, and this form of eyelid disease progresses markedly if left untreated.
- Spastic - occurs only on the lower eyelids. It occurs from constant inflammation of the mucous membrane in combination with contraction (spasm) of the retractor of the eyeball. The cause of spastic entropion may be a decrease in the palpebral fissure, the cause of which was surgery or the application of a tight bandage on the eyes. Spastic entropion may be almost invisible at a quick glance at a person. The deformation is visible only when the eyeballs move and with a certain position of the eyes (if they are deep-set).
- Senile - can appear in older people who have severely weakened muscles and cartilage that hold the eyelids in a normal position. With age, the skin stretches, the muscles become weaker - as a result, the eyelash edge turns inward. Entropion is more common in the lower eyelids of both eyes.
Entropion of the lower eyelid is diagnosed more often than the upper eyelid (the causes of the disease do not affect the statistics). This happens because the cartilage on the lower eyelids is almost twice as weak and smaller as compared to the upper ones. That is, they are easier to injure and more vulnerable to deformation.
Features of the eversion of the upper eyelid
The upper eyelid is generally less prone to eversion, which is due to its anatomy, since the cartilage on the upper eyelid is twice as thick as the lower eyelid.
Dense and powerful cartilage serves as excellent protection against deformation of the upper eyelid.
When the upper eyelid turns outward, deformation of the ciliary edge occurs. This type of pathology of the upper eyelid is more common in older people due to the weakening of the eye muscles. In this case, patients feel discomfort, as well as a constant feeling of sand or a foreign body in the eye. At the same time, the eye becomes red and irritated, the eyelid swells, and constant tearing occurs.
Vision with pathology of the upper eyelid becomes blurred. As the diagnosis worsens, keratitis develops, which can cause clouding of the corneal layer.
Diagnosis of ectropion
Ectropion of the century is easy to recognize on your own. During examination, the ophthalmologist confirms the diagnosis, identifies signs of complications, and establishes the causes and form of the pathology.
The type of pathology is determined by the results of an external examination and mechanical manipulation of the eyelid: for example, with cicatricial ectropion, scars from tissue damage are visible; the eyelid can be returned to the anatomically correct position if the skin is pulled to the side.
Most neoplasms can also be seen with the naked eye.
Paralytic ectropion is additionally indicated by a decrease or complete loss of sensitivity in the skin around the eyes.
Horizontal weakness of the eyelids can be detected by pulling the skin 8 mm away from the eyeball in the middle of the eyelid. In this case, the skin will return to its original position only after blinking.
Weakening of the lateral (outer) angle is recognized by the rounded shape of this part of the palpebral fissure. In addition, the outer corner can be pulled inward by only 2 mm.
Weakening of the medial (inner) angle can be determined by pulling the lower eyelid outward. With a slightly pronounced ectropion, the lowest point touches the limbus, with a more significant eversion - the pupil of the eye.
Diagnostics
Ectropion of the eyelid can be suspected based on the appearance of characteristic changes and clinical symptoms. The severity of changes is assessed by an ophthalmologist during an examination. It also establishes or excludes the development of relevant complications. To determine the cause of the changes, an additional examination is prescribed, which may include various methods of laboratory, instrumental and functional research.
Based on all the results of the diagnosis of the pathological condition, the doctor makes a conclusion and selects the most optimal treatment.
Clinical manifestations
The formation of symptoms of ectropion of the eyelid is caused mainly by a violation of the mechanism of outflow of tear fluid. It participates in the metabolic processes of the eyes, moisturizes the conjunctiva of the eyes, protecting it from drying out, and protects against the ingress of foreign particles. Tears are produced in the required volume by the corresponding glands, the ducts of which open mainly under the upper, and in small quantities under the lower eyelids.
Renewal and the impossibility of lacrimation (in the absence of emotional reactions) are ensured by the constant circulation of tears along the lacrimal ducts. Excess fluid enters the lacrimal sac through the lacrimal openings, located at the inner upper and lower parts of the eye, and from there through the nasolacrimal canal into the nasal cavity.
The above causes of the disease lead to lag of the ciliary edge (usually the lower one), drying out and irritation of the conjunctiva, which in turn causes additional production of tear fluid and its accumulation due to displacement of the lacrimal punctum or cicatricial deformation of the outflow tract. The prolonged existence of an eversion of the eyelid gradually leads to keratinization and thickening of that part of the conjunctiva that is tightly fused to the cartilage of the eyelid. At the border between them there are additional lacrimal glands.
The outflow of 90% of the tear fluid passes through the lacrimal punctum located on the lower eyelid, which is what causes the main clinical manifestations of ectropion in these areas:
- Continuous tearing.
- Frequent blinking due to a constant sensation of a foreign body, “sand” in the eye.
- The symptoms of conjunctivitis are the presence of injected (dilated) vessels, redness of the eye and a moderate burning sensation associated with irritation during constant mechanical removal of tears and the development of infection.
- Redness and maceration of the skin under the eye.
- Further development of symptoms of keratitis with subsequent clouding of the cornea and a significant decrease in visual acuity.
The severity of symptoms depends on the above reasons that caused the pathological condition and its severity. The latter is characterized as weakly expressed if there is only a loose fit to the conjunctiva of the eyeball, and significant - with a visually noticeable eversion of the mucous membrane, which can be approximately 1/3 of the eyelid (partial eversion) or along its entire length (complete eversion).
Blepharoplasty: indications and contraindications
It is important to understand that blepharoplasty is a surgical intervention, usually of a cosmetic type, but it can also be of a therapeutic nature. The operation is performed to change the shape of the eyelid, helps eliminate its overhang, and relieves the patient of ptosis.
Experts identify the following indications, in addition to the overhanging upper eyelid, for blepharoplasty:
- the patient has large bags under the lower eyelids;
- severe form of blepharoptosis, in which a person experiences discomfort;
- the appearance of severe dark circles under the eyes (it is important to remember that this symptom is characteristic of many diseases, so you first need to establish the cause of its occurrence);
- wrinkles at the outer edges of the eyes.
Before the operation is performed, the doctor identifies the causes of ptosis. For example, the congenital form of the pathology looks symmetrical, and its cause is abnormal muscle development. Therefore, as a consequence, “lazy eye” syndrome appears. If blepharoptosis of the upper eyelid is acquired, it is usually the result of a muscle strain, injury or nerve disease.
Contraindications in the presence of which blepharoplasty should not be performed include:
- pronounced pigmentation of the skin in the area around the eyes;
- tattooing in the eyelash area;
- systemic diseases during the period of decompensation;
- acute forms of inflammatory diseases of any origin;
- menstrual period in women.
Treatment of ectropion of the eyelid
Treatment may be:
- Conservative or symptomatic.
- In the form of a full-fledged surgical correction - blepharoplasty for eversion of the eyelid.
Conservative therapy
It is shown only when:
- weak severity of the defect;
- presence of contraindications for surgical treatment;
- the need to treat the underlying disease (paralysis or paresis of the facial nerve, damage to connective tissue due to systemic autoimmune diseases, tumors in the orbital area, etc.), which is the cause of ectropion; in this case, the result of treatment of the underlying pathology is the spontaneous elimination of eversion of the mucous membrane.
How is the operation performed?
Surgical treatment of eyelid inversion is performed under local anesthesia - anesthetic drops are instilled into the eye, and a local anesthetic is injected subcutaneously.
The doctor makes a small incision at the outer commissure of the eyelids (outer corner of the eye). The lower eyelid is pulled up in the temporal direction and secured with sutures. After surgery, an antibacterial drug is placed under the eyelid, and a cooling bandage is attached to the eye.
The total duration of the procedure is 60 minutes.
No hospitalization required. The patient is immediately released home after the operation.
Medicines to relieve symptoms
Additionally, in order to alleviate the unpleasant symptoms of entropion, the doctor may prescribe the following medications:
- Moisturizing drops: Visine, Systane, Lacrisify, Vidisic, Hilo-Komodo, Lacrisin, natural tear. They restore the integrity of the tear film and eliminate irritation of the mucous membrane. Usually available in the form of eye drops.
- Keratoprotectors: emoxipin, Korneregel, blepharogel. Prevents the development of dry eye symptoms and restores damage to the surface of the cornea.
- Gels with dexpanthenol. Accelerates the healing of postoperative wounds.
The patient's condition can be temporarily alleviated by special patches that are glued to the skin and pull back the rolled-up eyelid. Most often they are used in the case of senile entropion.
Some patients with entropion prefer to use soft contact lenses because they prevent eyelashes from damaging the cornea.
Prevention of entropion
When treating entropion, it is necessary to adhere to the rules of hygiene and regularly rinse the conjunctival cavity with an antiseptic solution. Using antiseptic and vitamin ointment, you can prevent damage to the cornea. Care for your skin regularly, especially if the adhesive bandage causes irritation.
Traditional recipes for preventing entropion:
- Wash your eyes with tea twice a week; this drink perfectly relieves inflammation;
- To improve the mucous membrane and strengthen the skin around the eyes, wash your face with cold water every morning;
- Several times a week, apply fresh cucumber (circles) to your eyes for 15 minutes;
- Make compresses from linden infusion.
Is surgery necessary?
Surgery is the only treatment for entropion that can eliminate entropion.
There are a number of methods for treating different stages of entropion, all of which are surgical. This can be the application of sutures that pull the eyelid to its natural anatomical position, excision of a small strip of skin on the eyelids, changing the shape of the orbicularis muscle of the eyeball, etc. In each case, the technology is determined individually, depending on the form of the disease, its severity, and medical history.
There is only one radical way - surgery. Without it, you can relieve symptoms and slow down the development of entropion, but these are temporary measures.
It is impossible to cure eyelid entropion with medication: there are simply no drugs that will “force” the eyelash edge to take the correct position. Medicines make it easier to prepare for surgery and speed up recovery after it, but without surgery you will not be able to recover.
In order for the surgical intervention to be as effective as possible and recovery after it to be quick, it is worth using auxiliary methods (on the recommendation of an ophthalmologist):
- medications whose action is aimed at restoring the cornea. They form a natural protective film, which allows you to quickly restore all functions of the eyelids after surgery;
- patches used to mechanically move the eyelid into the correct position. They simply fix the tissue so that the eyelashes cannot come into contact with the eyeball. Physically it is not very comfortable and looks rather strange, but the method shows good effectiveness, especially in childhood;
- contact lenses-films allow you to create an additional barrier between the eyelids and the mucous membrane. The lenses are soft enough not to damage or irritate the cornea, but at the same time dense enough to prevent eyelashes from injuring the eyeball.
Symptoms of entropion
The development of entropion occurs quickly with acute manifestation of symptoms. Contact with the mucous membrane of the eyelashes immediately makes itself felt. It seems to a person that a foreign body has entered the eye. The following symptoms are also concerning:
- pain, burning, tingling, itching;
- conjunctival hyperemia;
- increased photosensitivity;
- dry eyes;
- lacrimation, which develops as a protective reaction to the drying out of the connective membrane;
- deterioration of image quality, diplopia.
When blinking, all these symptoms intensify. In this state, a person cannot work, read, or drive a car. Entropion causes severe discomfort, and if left untreated, contributes to the development of other dangerous pathologies in which the conjunctiva and cornea become inflamed.
Surgical correction of lower eyelid inversion
Surgical treatment is indicated for age-related changes, the presence of post-traumatic, thermal or chemical post-burn scars, complications of blepharoplasty performed previously (for aesthetic purposes), or the introduction of cheek implants, etc.
The operation for inversion of the lower eyelid consists mainly of removing scars, strengthening the muscular-ligamentous apparatus and/or restoring an area of tissue with a skin flap in case of its deficiency. For these purposes, various techniques and their modifications are used - operations according to Kunt-Szymanovsky, Blashkovich, Imre, Filatov, Ficke and others.
The choice of technique is made based on taking into account the degree of eversion of the mucous membrane, the area of excess skin, as well as on the basis of determining the degree of such signs as:
- horizontal weakness of the eye tissues, which is characterized by their failure to return to their original position after the central part has shifted from the eyeball by 0.8 cm or more;
- tendinous weakness of the medial canthus, which is determined by pulling the lower eyelid outward. In this case, the location of the lowest point is recorded. In the absence of pathology, the latter moves no more than 2 mm; with moderate weakness it reaches the edge of the cornea, with severe weakness - the pupil;
- tendinous weakness of the lateral canthus is characterized by its rounded shape, while it is possible to displace the lower soft tissues of the lower parts of the periorbital region in the medial direction (toward the nose) by more than 2 mm.
Symptoms
Eversion of the eyelid is almost impossible to confuse with another disease. Usually the patient himself notes that the skin lags behind the eyeball. In addition to external manifestations, the anomaly is accompanied by the following symptoms:
- The appearance of a “pocket” between the eyeball and the edge of the eyelid. The inner surface of the mucosa becomes visible from the outside. It is a thin edging of bright red color;
- It is impossible to completely close the palpebral fissure. The deviation causes discomfort when blinking;
- Increased and uncontrollable lacrimation. The reason lies in the loss of contact between the eyelid and the eyeball. As a result, the tear stream is not able to penetrate the lacrimal punctum. As a result, liquid accumulates in the area between the eyelid and the eye, pouring out;
- Irritation of the skin of the affected eyelid. It is caused by continuous lacrimation and mechanical irritation of the conjunctiva. The complication is associated with regular wiping of accumulated fluid and swelling of the eyelid;
- Feeling of a foreign object or sand in the eye. The lower eyelid does not cover the cornea during blinking, which causes it to dry out;
- Redness of the organ of vision due to inflammation of the conjunctiva. When ectropion develops, the mucous membrane becomes open and the natural process of self-cleaning of the eyes fails. As a result, the conjunctiva dries out and begins to thicken.
Return to contents
Features of the eversion of the upper eyelid
It is less prone to developing ectropion because it has thick cartilage that provides excellent protection against deformation. If an inversion of the upper eyelid occurs, the ciliary edge changes. This anomaly is usually diagnosed in elderly patients, as the eye muscles weaken.
| The person experiences discomfort. It seems to him that sand or a foreign object has gotten into his eye. The organ of vision becomes red and irritated, the eyelid swells, and there is constant and severe lacrimation. |
When the upper eyelid is everted, the sharpness of the eyes decreases, objects become blurred. If the pathology progresses, then keratitis (inflammation) appears, which can provoke clouding of the cornea.
Features of lower eyelid inversion
Ophthalmologists use the concept of “ectropion” exclusively to define pathology affecting the lower eyelid. Due to its anatomical structure, it is this element of the organ of vision that is most often affected by illness.
Eversion of the lower eyelid comes in two forms:
- Easy. The defect is insignificant, the lag from the eye is minimal. Approximately 1/6 of the entire eyelid is damaged;
- Heavy. Ectropion is visible to the naked eye. The mucous membrane of the visual apparatus is turned outward. In some cases, the defect extends to the entire eyelid.
| In severe forms of the disease, doctors usually diagnose “spastic eversion.” The anomaly is accompanied by inflammation of the conjunctiva and a decrease in visual acuity. |
If lower eyelid entropion occurs in a child
In infants under 1 year of age, bloat occurs quite often, and this does not always mean the presence of a genetic predisposition.
Due to age, the muscles that hold the eyelid in its normal position may simply not be fully developed. This does not mean that you will necessarily have to “cut”; you can often get by with a set of conservative methods:
- use a patch that will fix the eyelid in the correct position. The difficulty is that small children (this method is best used before reaching 1 year old) simply do not allow it to stick;
- use a special gel that will protect the cornea and minimize its damage by the deformed ciliary edge;
- use antiseptics that help maintain eye hygiene when they become sour. For this, herbal decoctions (pharmaceutical) or a weak solution of baby shampoo that does not irritate the mucous membranes are used.
The combination of these techniques in many cases gives positive results - the position of the eyelid is completely normalized, and surgery to remove the entropion is not required. In this case, a systematic approach and implementation of all the ophthalmologist’s recommendations play a key role.
The effectiveness of the measures taken (or ineffectiveness) appears at approximately 11-12 months of age, and the ophthalmologist makes a decision on the need and extent of surgical intervention.
Inversion of the lower eyelid in a child can also appear at an older age. It is important to diagnose entropion in time to avoid problems with vision, which develops in childhood.
One of the clearest characteristic signs of entropion is that the child begins to pull his chin up and raise his head to see some object (the field of view is significantly reduced due to interfering eyelashes).
Rehabilitation after blepharoplasty for ectropion of the eyelid
Rehabilitation measures coincide with the general instructions for the patient after blepharoplasty: instillation of eye drops with a moisturizing and antiseptic effect; wearing sunglasses and using sunscreen cosmetics; performing gymnastics for the eye muscles. Do not wear contact lenses. You need to sleep on high pillows.
Visiting a bathhouse, sauna, or solarium is contraindicated. Alcohol, cigarettes, coffee are excluded. Physical activity is limited.
These prohibitions and restrictions must be observed for two months.
Treatment
The type of treatment for ectropion is chosen by the doctor depending on the cause of the disease and its severity. Typically, all types of treatment for ectropion come down to the following methods:
- eliminating the cause of the pathology;
- symptomatic therapy;
- surgical treatment.
When surgery is not needed
Ectropion is not always treated promptly. In some cases, conservative treatment is sufficient. Indications for such therapy are cases when:
- symptoms are mild;
- there are contraindications for surgical treatment (age, drug intolerance, disease);
- It is enough to eliminate the cause of the disease (tumors, paresis of the facial nerve, etc.), and ectropion will go away on its own.
The usual practice of ectropion therapy is the prescription of procedures and medications that help alleviate the patient’s condition and avoid complications of the disease (conjunctivitis, corneal ulceration, etc.). With this method of treatment, the following methods are often used:
- using a special patch at night to facilitate closing the eyes (if not closed);
- inclusion of drugs to moisturize the mucous membrane of the eyeball (usually such as artificial tears) for instillation several times a day;
- stitching the edges of the eyelids to protect them from drying out (in severe cases of the disease).
Surgical treatment of eyelid inversion
Surgical treatment is indicated mainly for the following types of ectropion:
- senile;
- cicatricial;
- mechanical (after getting rid of the tumor that caused the eyelid change).
The surgical technique is selected taking into account the patient’s age, the condition of the body and eye tissues.
The main points are:
- the reason for this inversion;
- the presence of scars;
- the degree of elasticity of the ligaments supporting the corners of the eyes.
- condition of soft tissues, their excess or deficiency (after blepharoplasty for the purpose of rejuvenation).
Surgery for ectropion is always performed by an ophthalmologist or plastic surgeon.
The essence of the operation for ectropion is to return the deformed eyelid to the correct position and fix it.
Before the operation, the patient needs to consult a surgeon and conduct a number of studies:
- blood (general, coagulation and biochemical analysis);
- urine (general analysis);
- ECG;
- chest x-ray.
Typically, surgery for ectropion is performed under general anesthesia, so before the intervention you need to consult an anesthesiologist.
Sometimes consultations with doctors of other specialties and additional tests may also be necessary.
Surgery for ectropion
The operation for eversion of the eyelid lasts from one to three hours, depending on the complexity and technique used. In addition to correcting the external defect, this operation normalizes the process of tear drainage and eliminates the cosmetic consequences of ectropion (hernias and excess skin are removed from the eyelids, the outer corners of the eyes are raised). Such additional points are clarified in advance if the operation is performed by a plastic surgeon.
Incisions in such operations are placed in natural folds of the skin using a cosmetic suture. Subsequently, postoperative scars are completely invisible.
For several weeks after the intervention, hematomas and swelling of the eyelids and parts of the face will persist. Already in the first hours after surgery, cooling compresses are used to reduce swelling.
We advise you to read: PTOZ can develop under the influence of many reasons and is a cosmetic defect that can be treated therapeutically.
Inpatient observation is required on the first day of the postoperative period.
After discharge, patients are scheduled to visit the attending physician to monitor the tissue healing process.
Physiotherapeutic procedures (usually in combination with proteolytic enzymes) are often used to speed up postoperative recovery and resolve scars.
Contraindications for surgery
Surgical treatment of ectropion has its contraindications. It is often impossible to use surgery for ectropion in older people. Also, such contraindications may be serious pathologies associated with:
- diseases of the heart and blood vessels;
- hypertension with frequent crises;
- complicated by diabetes mellitus;
- severe thyroid diseases;
- retinal detachment;
- dry eye syndrome.
Negative consequences of the operation
Sometimes it is not possible to completely eliminate the defect with ectropion. And after the operation itself, a narrow gap remains between the eyeball and the edge of the eyelid. As a result, the risk of re-development of the eyelid gate remains high.
Common postoperative complications with this disease may also include manifestations associated with:
- wound infection;
- divergence of seams;
- bleeding from a postoperative wound;
- the appearance of cysts in the epidermis;
- dysfunction of the lacrimal glands;
- blepharoptosis (drooping of the upper eyelid);
- lagophthalmos (inability to close the eye).
An unpleasant surprise for patients is that to eliminate all of the above complications, they often have to undergo a second operation.
Memo for the patient after ectropion surgery
To minimize the risk of complications after ectropion surgery, the patient during the recovery period is usually advised to:
- refusal of any visits to baths, saunas and generally thermal procedures on the face for 2 weeks (to reduce swelling and bruises);
- limiting any physical activity and avoiding bending for 1 month (for successful resorption of swelling and tissue restoration);
- protection from direct sunlight to the eyes (including avoiding visiting a solarium) for 6 months (to prevent the appearance of unnecessary pigmentation on the eye).
Any eye disease should alert you. The visual organ is not only extremely important for a full life, but also requires special attention: “Take care of your eye like a diamond!” Eversion of the eyelid is not only a cosmetic defect, but also provokes many visual disturbances. For effective treatment of this disease, it is especially important to correctly determine the cause of its occurrence. Often, to eliminate this eye pathology, surgical treatment is required, after which it is important to comply with certain restrictions. A professionally performed operation helps eliminate all symptoms of eyelid inversion and avoid its various complications. Take care of your eyes!
Sources used:
- Secrets of people who see well / Oleg Pankov. - M.: AST, 2014.
- Skoromets A. A. Topical diagnosis of diseases of the nervous system: A guide for doctors. — 1st ed. - L.: Medicine, 1989
- How to restore vision without surgery / Marina Ilyinskaya. - M.: Eksmo, 2020.
- National Eye Institute
Forecast
With timely initiation of therapy or early blepharoplasty, provided that all postoperative recommendations are followed, the prognosis of the disease is quite favorable. The cosmetic defect is eliminated, visual acuity is restored, and the patient returns to a normal quality of life. However, in the case of severe pathology, the risk of relapse cannot be excluded.
Ectropion of the eyelid is a pathology that is not only a cosmetic defect, but also causes severe discomfort and can lead to partial or complete loss of vision. Modern treatment methods are effective and can prevent dangerous complications. Sometimes ectropion of the eyelid goes away on its own after treatment of the underlying disease. However, in most cases, patients require surgery.
Ectropion correction (video)
Prevention and prognosis
If the treatment was timely, the lower eyelid inversion goes away without aggravating consequences, so the prognosis is favorable. The addition of a secondary infection can lead to deterioration of vision, pathological changes in the iris, conjunctiva, and cornea. To prevent ectropion from occurring, you should eat properly, including foods containing collagen in your menu, and do exercises for the eye structures. It is not recommended to overuse cosmetic procedures, and before manipulating the eyelids, you should consult a doctor. It is also necessary to thoroughly clean the visual organs.