Tubular breast plastic surgery is one of the most popular plastic surgeries, the task of which is to restore the usual anatomical shape of the mammary gland. Features of “tubularity” are the absence of a pronounced lower pole of the breast; the main concentration of the mammary gland is observed around the nipple. During the operation, the configuration of the gland is completely changed. Correction of tubular breasts is carried out solely at the request of the patient; this structure of the mammary gland does not affect the main function of feeding; the operation is performed for aesthetic reasons.
What is tubular breast shape, signs
The tubular form of the mammary glands is a developmental anomaly, against which the area of the base of the breast decreases , mastoptosis, alveoreal hernia and connective tissue deficiency develop. The glands acquire a characteristic elongated tubular shape.
There are unilateral and bilateral lesions, the areolas protrude slightly. The pathology is diagnosed in 20-25 patients out of 1000. Patients rarely seek medical help due to the fact that the disease is practically asymptomatic. Pathology is considered an aesthetic defect.
An anomaly is detected during external examination. Depending on the degree of damage, the chest has a cylindrical or cone-shaped shape. At the base, the organ narrows, the interthoracic space is enlarged.
It is possible to develop glandular ptosis. The mammologist often discovers that the areolas are underdeveloped; they are dilated and do not correspond to the patient’s age. The nipples are dense, structural anomalies are observed (for example, retraction).
In rare cases, an alveolar hernia is diagnosed, which is manifested by protrusion of the nipple complex. There are no subjective symptoms manifested in the form of discomfort or pain.
When breastfeeding, the tubular shape of the breast can become an obstacle for the baby to latch on to the nipple.
A woman may experience difficulties during breastfeeding caused by a decrease in the volume of the mammary gland.
The child cannot latch onto the breast correctly if the structure of the areolar-nipple complex is abnormal.
Causes of tubular breasts
The tubular form of the mammary glands develops for a number of reasons.
Scientists have put forward several theories about the occurrence of pathology:
- Acquired factors. A number of researchers do not consider the pathology to be congenital due to the absence of changes in the areolar-nipple complex until adolescence. The reason for the development of the tubular form, in their opinion, is a violation of blood flow inside the mammary glands.
Tubular breast form can develop during adolescence
- Teratogenic factors. The anomaly occurs against the background of a biological or chemical effect on the fetus developing in the womb.
- Hereditary factors. Tubular breasts can be passed down the female line from mother to daughter. The key genes that are responsible for the development of the disease have not yet been identified.
With “goat breasts”, dense bridges are formed inside the mammary glands (one or two), preventing the normal growth of glandular and fatty tissues.
Tubular breasts after childbirth
The tubular form of the mammary glands cannot develop during pregnancy or while breastfeeding.
An aesthetic defect cannot be considered acquired. Pathology is not an absolute contraindication to lactation. Women suffering from grade 2 or 1 anomaly can breastfeed their baby.
An aesthetic defect does not in any way affect the quantity and quality of milk. Women with grade 3 may have trouble latching on to the baby's areola and nipple. The mother must choose the right position during feeding so that air does not enter the baby's stomach. Breast deformation does not affect lactation in any way.
Tubular breasts in a teenager
The tubular form of the mammary gland in adolescents appears during puberty. The number of glands in the chest increases 8-12 times. Tubular lobes are intensively formed.
Only a mammologist can determine the presence of pathology in adolescents.
A mammologist can confirm or refute the diagnosis after the mammary gland is fully formed. The development of pathology is in no way connected with maintaining strict diets: the disease is inherent in a person from the moment of his birth
Stages of tubular breast surgery:
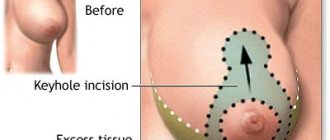
- The surgeon makes 1 or 2 incisions around the circumference of the areola and, if necessary, reduces it.
- Breast lift along the areola (an additional vertical incision can also be performed).
- The doctor creates a “pocket” for the implant, redistributing the breast tissue.
- Installation of implants.
- Stitching.
The tubular breast after plastic surgery retains sensitivity and functionality, if the operation is performed correctly. In the photo of the tubular breast before and after surgery by an experienced surgeon, the difference between the initial result and the result of the work of a mammoplasty specialist is clearly visible.
Types and degrees of tubulation
Tubular breast cancer is not considered a life-threatening condition. The disease does not require urgent mammoplasty. The gland is usually shaped vaguely like a mushroom. There are several main degrees of tubulation.
Among them, the type of disease characterized by:
- cone-shaped and tube-shaped;
- predominance of vertical size over horizontal;
- small base of the mammary gland;
- deficiency of breast volume.
Tubular form of the mammary glands: degrees
The lower part of the breast is narrowed, the areolas and nipples are drooping. There is pronounced asymmetry.
Initial degree
Stage 1 tubulation of the mammary glands is considered the mildest form that does not require correction. The aesthetic defect is mild: the breast is slightly raised, the areolar-nipple complex is not changed.
The growth of the mammary gland is hampered by the formation of bridges formed from connective tissue. They are located in the lower and medial quadrants.
Second degree
In the second degree, tissue deficiency is formed in the lower quadrant. The mammary gland is slightly lowered or displaced downwards. During a visual examination, thickening of the nipple and expansion of the areolar lobe can be detected.
Third degree
Stage 3 tubulation is considered the most severe. In a woman, a sheath of connective tissue forms inside the mammary gland, narrowing the glandular base and preventing its growth. There is a shortage of tissue. There is a high risk of developing alveolar hernia.
Tubular form of the mammary glands of the 3rd degree threatens the development of alveolar hernia
Due to the sharp expansion of the areola-nipple complex, the breast grows towards the nipple. In the third degree, experts recommend choosing an implant to eliminate the defect.
Causes and types of pathology
The initial reasons that influence the formation of tubules are still not clearly determined. At the same time, medical research has been going on for several decades, namely since 1976. It has been precisely established that the presented algorithm is associated with a defect in the formation of the mammary gland. The point is that a powerful frame made of connective tissue prevents it from straightening in all directions, as well as from developing to its full extent. Features of fibrosis.
The result of this is that the mammary gland grows exclusively in the nipple area. As a result, the areola protrudes, stretches, and often leads to a periolar hernia. The areola itself remains developed, but not completely. Experts distinguish three categories of breast development in this case:
- the first type of condition is closest to the usual development of the mammary gland and does not need correction. A slight degree of underdevelopment is identified, which refers to the inner and lower region of the mammary gland. The breast turns out to be minimally raised up, and the nipple is lowered down,
- the second type of condition is identified by tissue deficiency in the thoracic region, namely in the lower region. In the vast majority of cases, it moves down, the nipple remains flat, and the areola is sufficiently enlarged, similar to the photo,
- the third type of tubularity is characterized by a significant deficiency of glandular tissue. The condition is characterized by a small area, which is combined with a flat nipple and stretched areolas. In the vast majority of cases, this is precisely this type of pathology in the formation of the mammary glands, which in patients is associated with significant discomfort not only in personal, but also in intimate life.
In order to have an even more complete understanding of what tubular breasts are, it is necessary to become familiar with the symptoms. In addition, this is what will allow you to identify the pathology from the photo.
Methods for correcting breast shape, indications
A woman with tubular breasts must make her own decision about the need for surgical intervention.
Specialists offer patients with mild forms of the disease a lift. Endoprosthesis replacement or mammoplasty is indicated for grade 3 tubulation. Breast prosthetics refers to improving the shape and increasing the size due to the revitalization of the implant in the tissue.
A breast lift is an operation during which endoprostheses are not installed. After surgery, the geometry of the mammary glands changes, sagging is eliminated and the correct shape is formed. The main indications for mammoplasty include not only tubulation, but also ptosis.
The disease is considered a complication of “goat breast”, due to which the tissues that form the mammary gland are stretched. There are 1, 2 and 3 degrees. Pathology is detected by visual examination: the mammologist pays attention to the location and size of the nipple.
There are several main methods of tightening. They are distinguished by the volume of tissue to be cut and the geometry of the incisions. The rehabilitation period and the duration of the operation directly depend on the complexity of the surgical intervention.
Mammoplasty or endoprosthetics is indicated for tubular breasts of the 3rd degree
A semi-monthly lift is indicated for women with moderate deformities of the mammary glands (1-2 degrees of tubulation). An incision is made on the falciform lobe, capturing the upper areolar semicircles.
After the operation, the breast takes on the correct shape, and the nipple is moved to the right place. Periareolar mastopexy involves an incision along the contour of the pigment spot. Scars after such operations are almost invisible.
To eliminate significant deformations due to tubulation or grade 3 ptosis, a long incision is made from the areola to the inframammary fold. Endoprosthetics is also very popular.
Breast correction surgery
There are several methods for correcting the shape and size of the mammary gland, but doctors believe that installing implants will be the best option - less traumatic and with a stable result. Another advantage of installing an implant in the mammary glands is that the structure of the tissues and milk ducts does not change, so the woman will be able to breastfeed her child in the future.
Algorithm for performing breast correction surgery:
- The surgeon opens access to the areola (the pigmented area around the nipple) and makes two circular incisions. If there are indications, the doctor immediately reduces the size of the areola.
- Tissue detachment is carried out, which allows the formation of a “pocket” for the implant. The dimensions of this space are agreed upon in advance with the patient and depend on what size breasts the woman would like to see in the future.
- An implant is inserted into the formed “pocket”. Drainage must be done - a narrow tube with a vacuum is fixed to the side of the mammary gland, through which blood clots will come out in the first 1 or 2 days after the operation.
- The surgeon connects the edges of the wound and sutures it in two stages. First, internal sutures are applied with special self-absorbing threads. Then the external seams are made exactly according to the previously made markings.
- Cosmetic stitches are applied. They make it possible to make traces of surgical intervention almost invisible and finally fix the edges of the wound.
Watch the video about the procedure for tubular breast surgery:
The duration of the operation is maximum 2 hours. Often, instead of artificial implants, doctors use the patient’s own fat tissue, in which case the intervention will be classified as lipolifting. This method of solving the problem of tubular breasts has undeniable advantages:
- the material is not rejected, as it is natural and is adequately accepted by the body,
- the rehabilitation period proceeds quickly and without complications,
- an allergic reaction does not develop.
The doctor should warn that adipose tissue can be absorbed over time, so lipolifting will have to be done in a few years. In addition, it is impossible to increase breast size by several points in this way.
Contraindications and consequences
Surgical interventions for the tubular form of the mammary gland have a number of contraindications.
Mammoplasty cannot be used during pregnancy and breastfeeding.
These include:
- period of pregnancy and breastfeeding;
- benign and malignant neoplasms in the breast area;
- childhood or adolescence (up to 18 years).
Mammoplasty can be considered a safe procedure. The operation must be performed by a highly qualified specialist in compliance with all standards of asepsis and antiseptics.
The consequences that arise after endoprosthetics include:
- Pathological swelling. Most often, tissue swelling goes away on its own within 3-5 days after surgery. If a woman is plagued by severe pain, temperature fluctuations, local low-grade fever, and hyperemia are observed, then it is necessary to consult a doctor as soon as possible.
- Gray. In this case, lymphatic fluid accumulates in the subcutaneous fat. The condition can be triggered by non-anatomical tissue dissection.
Signs include redness of the scar, severe aching pain in the incision area, discharge of clear fluid from the scar, and severe swelling. In case of serous syndrome, drainage or dissection of the wound is necessary, followed by pumping out the fluid.
- Subcutaneous hemorrhages. Due to unqualified actions of the plastic surgeon, improper stopping of bleeding or tissue injury during excision. Small hematomas are considered normal; they disappear on their own after 5-7 days.
Extensive hematomas that affect the armpit area and shoulder indicate the need to consult a doctor. Most often, patients complain of severe pain and fever. The doctor must first stop the bleeding.
Breast sagging occurs when the implant size is incorrectly selected
- Sagging breasts. A complication occurs when the implant size is incorrectly selected. It forms after 3-6 months. after operation.
Sagging can be pronounced and artificial (if a woman has a small prosthesis installed, then the breasts sag or the body reacts to a foreign body in this way). The defect can be corrected only with repeated mammoplasty.
- Implant contouring. Complications are detected in women who have a thin subcutaneous fat layer. In this case, the contours can be visible through the skin. Characteristic symptoms include unnatural protrusion. Corrective fillers that are injected into the mammary gland will help correct the situation.
- Suppuration. This is the most dangerous complication that occurs against the background of non-compliance with the rules of antisepsis and asepsis. Women complain of redness, temperature fluctuations, severe swelling and pain.
Pus may drain from the nipple or surgical scar. It is easiest to stop inflammation at the initial stage through antibacterial drugs and antieptics. In advanced cases, repeated surgery is required.
- Capsular contracture. Connective tissue forms around the implant. If growth occurs incorrectly, capsular contracture occurs. The breasts become deformed, when palpated, dents and lumps are revealed, and the woman experiences severe pain.
Stage 1-2 contracture is eliminated with the help of anti-inflammatory drugs, massage and physiotherapy. Stage 3-4 can only be corrected through surgery.
- Skin rash. Ripping is characterized by the formation of folds that vaguely resemble fingerprints. The defect is most noticeable when bending. The condition develops against the background of an incorrectly sized implant. To eliminate it, lipolifting is used.
To minimize the risk of complications after surgery, it is necessary to contact highly qualified specialists who have the appropriate certificates and diplomas.
Stages of surgery to correct tubular mammary gland
Surgical interventions on the female breast are considered one of the most complex plastic surgeries. The procedure should be carried out by a specialist who has extensive experience in this field and intuitively understands the problem. Each anomaly is individual, so an integrated approach is important.
The operation includes four stages:
- correction of the shape of the mammary gland;
- mammoplasty (implantation of hydrogel or silicone implants);
- moving the areolar-nipple complex to the desired point;
- formation of the inframammary fold.
During surgery, the specialist must eliminate the periareolar hernia (if present) and correct the asymmetry of the mammary glands, reducing the interbreast space.
Selection of implant
Before the operation, the specialist must agree with the patient on all stages of the surgical procedure.
Endoprostheses should be selected as high quality as possible, meeting the following criteria:
- Low risk of rupture. It is recommended to select the most durable implants that do not break due to injuries or falls.
- Safety. Almost all fillers present in dentures are completely safe for women.
- Biocompatibility. The main component is a gel, which remains in place when cut. The implants are made of modern materials, so the prostheses take root well in the woman’s body.
For tubular breasts, hydrogel or silicone implants are implanted.
The first contains:
- Highly cohesive gel. Dense material does not leak when damaged, the risk of rupture is minimal.
- Cohesive standard gel. The consistency resembles jelly. If the prosthesis ruptures, the gel dissolves in the body on its own.
Bioimplants contain carboxymethylcellulose, a natural polymer of natural origin. The substance is completely safe for the human body. When a prosthesis ruptures, carboxyl methylcellulose breaks down into carbon dioxide, water and glucose.
After implantation, a woman can examine her breasts using x-rays: the implant transmits x-rays well. Today, prostheses with a smooth surface texture are rarely implanted.
For tubular breasts, implants with a textured surface are used. They are not overgrown with connective tissue, which minimizes the risk of complications after implantation.
There are drop-shaped (anatomical) and round. Prostheses belonging to the first category are suitable for women suffering from ptosis or tubular form of the mammary gland of the 3rd degree. The structure of these dentures is quite dense, so they retain their shape well.
When choosing a prosthesis, the doctor must take into account the individual structural features of the patient’s body:
- breast density;
- body proportions;
- sternum size (hypersthenic, normosthenic, asthenic);
- elasticity of the skin;
- natural breast size.
After receiving all the data, the doctor conducts an analysis and selects the most suitable implants in terms of volume and shape.
Prosthetics
The implant is implanted in 2 quadrants: in the lower part of the breast (under the mammary gland) or in the upper part of the breast (under the pectoral muscle). The specialist makes a tissue incision along the border of the areola and pushes the skin flaps apart. The bridges that interfere with the growth of the mammary gland are cut off.
An implant is implanted into the space created after these manipulations. After installation of the endoprosthesis, the blood that has entered the cavity is removed. The fabrics are slightly stretched and stitched together, and cosmetic stitches are applied to the surface.
Mammoplasty: options for implantation
If a woman has small breasts or the skin does not stretch well, then after excision an expander must be installed in the cavity to facilitate tissue stretching. It must be regularly pumped up with solution. Stretching is carried out for 5-8 months. This is the safest and most painless method.
Breast lift (mastopexy)
Mastopexy is an operation to restore the shape of the breast.
The procedure has contraindications, which include:
- eczema at the incision site or pustular lesions of the epidermis;
- the period of bearing a child and breastfeeding;
- psychosomatic diseases;
- the presence of malignant and benign tumors inside the mammary gland;
- diabetes;
- poor blood clotting;
- severe pathologies of internal organs (including renal, liver and heart failure);
- cysts, mastopathy, cicatricial changes in the gland;
- acute infections.
Mastopexy or breast lift is contraindicated in case of mastopathy.
Before the operation, the patient must undergo a series of studies and consult with specialists (gynecologist, neurologist, cardiologist, therapist).
She may be assigned:
- electrocardiogram;
- mammography or ultrasound;
- tests for syphilis, hepatitis and HIV;
- General analysis of urine and blood.
14 days before the proposed operation, the doctor must completely stop hormonal and blood-thinning medications. A woman should get rid of bad habits (smoking, drinking alcohol) in advance.
Types of mastopexy
Breast lift is performed in several ways:
- mastopexy with implantation;
- periareolar mastopexy;
- vertical mastopexy.
The operation includes several stages:
- the skin is treated with an antiseptic;
- make a cut along the lines outlined in advance;
- Excess skin is excised and the nipple is moved to the desired point;
- apply a cosmetic suture;
- treat the skin with antiseptics;
- cover wounds with napkins.
Anchor breast lift
If there is blood left inside the cavity, it is necessary to install a drainage that will ensure the outflow of biological fluid. Types of mastopexy are distinguished by the size and location of the incision. During the operation, excess skin is excised, the edges of the wound are sutured together, and a cosmetic suture is applied.
Stage 3 breast tubulation can be corrected with an anchor or vertical lift. The incisions are placed under the breast or near the nipple line. The operation is considered complex - it leaves more scars compared to other surgical interventions.
Rehabilitation period after plastic surgery
If the operation was successful, the patient is discharged 24 hours after surgery. During this time, specialists will once again examine the woman and identify possible complications. After discharge, you must follow a number of recommendations to speed up the wound healing process.
You can’t spend a lot of time lying down; it’s better to rest while sitting or reclining. Food can be taken no later than 5 hours after surgery, and water - after 3 hours. Cold compresses will help relieve pain.
After mammoplasty, it is recommended to rest sitting or reclining
You can take a shower on the 5th day after surgery. The seams are pre-sealed with adhesive tape. You cannot wash your hair yourself : for 30 days you must limit your hand movements.
The bath is taken 6 weeks after surgery. In the first 7-10 days after plastic surgery, the patient should take analgesics and anti-inflammatory medications. During this period, the risk of side effects is high. Diarrhea or constipation usually goes away on its own.
Sutures are removed 14-16 days after plastic surgery. It is recommended to abstain from sports and intimate relationships for 10-14 days. People return to physical activity gradually, 30-35 days after plastic surgery. It is strictly forbidden to consume alcohol and tobacco products for 45-60 days after surgery.
Rehabilitation
After the operation, the woman remains in the clinic for a day under the supervision of doctors. To reduce pain, special painkillers are prescribed. The next day after surgical procedures, the surgeon performs the first dressing. The first days you should sleep on your back, and remove the bandage only a week after the plastic surgery.
Upon discharge, the surgeon gives the patient a sheet of recommendations that must be strictly followed during the rehabilitation period. After surgical treatment it is necessary:
- refuse heavy physical activity;
- visit the clinic for dressing changes;
- for six months do not visit the bathhouse or sauna, do not take a hot bath;
- Avoid exposure to direct sunlight, avoid solariums;
- wear compression garments (1-2 months);
- perform light exercise to improve wound healing (prescribed by your doctor).
After the operation, normal activity begins already on the 3rd day. 2 weeks after plastic surgery, a woman can return to everyday life.
Among the special medical recommendations: ultrasound of the mammary glands - annually, follow-up examinations with a doctor - at 3.6 weeks, 3, 6 and 12 months after surgery.
Cost of correction
The cost of the operation may vary depending on the type of tubulation and the severity of the defects.
Approximate prices:
| Type of intervention | Price |
| Mammoplasty (endoprosthetics) | 120,000 – 240,000 rub. (including the cost of prostheses) |
| Periareolar mastopexy | 165,000 – 245,000 (excluding cost of prosthesis) |
| Vertical mastopexy | 210,000 – 220,000 (without implants) |
| Anchor mastopexy | From 240,000 rub. |
The total amount includes the cost of consultation, examination, anesthesia and the implants themselves. If a complex intervention is planned, the patient will need to pay for her hospital stay.
Alternative options for breast correction
You can correct the shape of your breasts without resorting to surgery. Alternative methods may help women with mild tubularity.
If the defect is barely noticeable, the specialist prescribes a number of physiotherapeutic procedures to the patient:
- Microcurrents. The procedure stimulates metabolism, accelerating the process of collagen production. Under the influence of microcurrents, skin elasticity increases.
- Myostimulation. During the session, an electric current is applied to the pectoral muscles. It increases the onus of the pectoralis minor and major muscles.
At home, you can perform a number of exercises on your own to restore the shape of your mammary glands.
Exercises to restore the firmness of sagging breasts
A set of exercises to tighten the pectoral muscles and restore the shape of the mammary gland:
- Bench press.
You need to lie down on a bench with your feet on the floor. Take dumbbells in your hands. Bend your right and left arm at the elbow and lift it up. Fix the position. You need to perform 4-5 sets of 10 repetitions per day.
- Push ups. Perform from a lying position on the floor or leaning against a wall. When doing push-ups, your arms must be fully straightened. The exercise is repeated 4 times, performing 10 approaches.
- Palm press. Stand leaning against the wall, bend your arms at chest level, placing your palms together. Inhale, hold your breath for 10 seconds and forcefully press your palms together. After 15 seconds, repeat the exercise. The number of approaches is 6-8.
You can tighten your chest only if the above exercises are performed regularly.
Cosmetology procedures
Cosmetic procedures can help correct tubular breast shape. Meso-cocktails and preparations containing hyaluronic acid are injected into the mammary glands.
If a woman has small breasts, then you can restore their shape using lifting threads:
- Aptos. The active ingredient is polylactic acid. There is no need to remove them; the threads dissolve on their own in the tissues. Participate in the formation of a framework of elastin and collagen.
- Mesothreads. The main component is polydioxanone, the coating is polyglycolic acid. Completely dissolve in 250-280 days.
- Platinum and gold threads. They are made of precious metals (999 standard, 24 carats). They do not dissolve on their own; after they become overgrown with connective tissue, they tighten.
During the implantation of threads, the patient is not put to sleep; she can observe the process. The procedure is completely safe and painless.
Tubular breast shape is corrected after puberty. Surgeries on the mammary glands are not performed in adolescence. The final result depends on the individual characteristics of the body - in some cases, implants take a long time to take root.
Preparation for plastic surgery
No specific preparation is required, but the patient should:
- undergo a full examination by specialized specialists - a cardiologist, endocrinologist, oncologist,
- 30 days before the appointed date, stop drinking alcohol and smoking.
It is important to adhere to a certain diet - sweets, fatty foods, and spices are excluded from the diet. The fact is that a woman’s body must be cleansed of toxins and waste - this will ensure rapid healing and tissue restoration in the postoperative period. In addition, 20, 30 days before the manipulation you need to stop using hormonal drugs and Aspirin.
On the day of surgery, the woman visits the surgeon who will perform the surgery. The doctor must make markings on the chest in order to understand where and how to apply stitches during the operation.