The human vascular system is simple, but it plays a very important role. The most important functions thanks to which a person can carry out any activity are based on it.
Zmist:
- Indications and contraindications
- Before angioplasty
- Operation technique
Unfortunately, blood vessels are subject to many negative influences, due to which they lose their strength, which undoubtedly affects human health.
Despite this, there is reason for joy: modern medicine has developed quite a lot of methods to combat these problems, and one of the simplest and most effective is laser angioplasty.
The very meaning of the word angioplasty suggests that the purpose of the operation is to restore the shape and plasticity of blood vessels. This method became known in the late 60s of the twentieth century, for which credit should be given to A. Grünzig, who introduced this method of restoring vascular functionality. Today it is quite widespread.
to the point ↑
Indications and contraindications
Most often, angioplasty is performed for those who have severe narrowing of the arteries or their blockage, which often occurs with atherosclerosis.
Many people know that atherosclerosis is a gradual process, which is characterized by the formation of plaques that clog and narrow the arterial lumen.
Arteries can be compared to pipes through which oxygen and blood are delivered to tissues and organs, so their blockage leads to disruption of this vital process.
This causes unpleasant symptoms.
For example, if there is a blockage in the artery of the lower limb, pain may occur both when walking and at rest. The blockage causes your blood pressure to rise. It is very important to resolve such problems in a timely manner to avoid further complications.
There are several diseases for which angioplasty is most often prescribed:
- IHD;
- renal artery stenosis;
- lesions of the carotid artery;
- peripheral vascular diseases.
Angioplasty using a laser is most often performed if balloon angioplasty is not possible. This method is effective for occlusions, plaques formed at the mouths of arteries and for extended and heavily calcified plaques.
There are several contraindications to the use of this method:
- thrombosis;
- bifurcation stenoses;
- damage to convoluted areas.
to the point ↑
Angioplasty and stenting of the carotid arteries
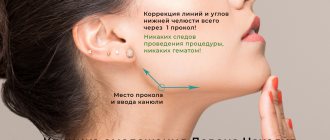
Carotid angioplasty is performed in cases of significant narrowing and blockage of the carotid arteries, after examination and diagnosis.
This technique is a procedure for introducing a catheter with a balloon into the vessels of the carotid artery, which reaches the affected areas of the artery and is inflated under high pressure. To achieve improved long-term results, it is recommended to supplement the operation with stenting, the most advanced and least traumatic method of treating carotid artery stenosis. The stent pushes the narrowed walls of the artery apart and keeps them straightened constantly.
Read also: Pulmonary edema in dogs
Stenting of the carotid arteries requires the use of a device to protect against distal embolization, which ensures that small arteries of the brain are not blocked by particles of crushed plaque during the stenting process.
Before angioplasty
In order for the procedure to be successful, certain measures must be followed.
- On the eve of the procedure, after 12 pm you cannot eat solid food, you can only drink water.
- You must continue to take medications. If the patient is taking insulin, it is necessary to consult with the attending physician about its dosage. You may need to stop taking antidiabetic medications two days before and two days after the procedure. Of course, during this period you should consult your doctor about your blood sugar levels. You should definitely tell your doctor if you are taking medications that reduce blood clotting, as you may also have to stop taking them for a while.
- If the patient is allergic to contrast agents or iodine used in angiography, be sure to inform the doctor about this.
- You should not smoke for 24 hours before surgery; it is best to give up this bad habit altogether.
Before angioplasty, an intravenous catheter is installed in one of the veins. This is done so that fluids and medications can be infused conveniently during the procedure. Dentures and jewelry should also be removed.
to the point ↑
Areas of application of angioplasty
Coronary angioplasty and stenting
Coronary angioplasty is performed to treat patients with coronary heart disease and acute myocardial infarction. Angioplasty is much safer than coronary artery bypass surgery in that there is no need to open the sternum, and the patient is released from bed rest after a maximum of two days. Percutaneous transluminal coronary angioplasty (PTCA) is widely used to repair coronary arteries. If necessary, special stents are installed after coronary angioplasty. Timely coronary angiography and angioplasty can save patients with a heart attack, but it must be performed as quickly as possible after an attack of angina.
Angioplasty of leg vessels
Balloon angioplasty is very effective for diabetic artery disease of the leg, especially diabetic foot and gangrene. Patients do not require any incisions, only a puncture is performed. In most cases, after angioplasty, the patient can be transferred or discharged the next day. Endovascular surgery allows you to perform complex operations to restore blood circulation in the legs, even in patients burdened with many concomitant diseases. In our clinic, most patients with iliac artery disease (Leriche syndrome) are treated without incisions, with angioplasty and stenting. Peripheral angioplasty of the leg arteries can be used with great success in diabetic foot with the development of gangrene.
Angioplasty and stenting of the carotid arteries
The simplicity and effectiveness of angioplasty has prompted vascular surgeons to use it in complex carotid surgery. The advantage is the absence of incisions and anesthesia, the speed of implementation, and the absence of the risk of damage to important cranial nerves. However, there remains a certain risk of developing cerebrovascular accidents, greater than when performing traditional open carotid endarterectomy. This risk is associated with the possibility of damage to the plaque during the passage of the guidewire and balloons, which can lead to the entry of plaque elements into the cerebral vessels. In our clinic, modern MOMA technology is used to prevent complications of carotid angioplasty, and special filters are used to prevent embolism.
Angioplasty of the renal arteries
Narrowing of the renal arteries leads to impaired renal function and malignant hypertension. Previously, operations on the renal arteries were performed very rarely, due to the large surgical incision, which was more dangerous than intervention on the vessel. With the advent of special balloons and stents, the treatment of narrowing of the renal arteries has become much easier. The effectiveness of renal artery angioplasty reaches 90%.
Removal of blood clots using Rotarex technology
The presence of acute arterial thrombosis against the background of large atherosclerotic plaques poses a major challenge in the treatment of such patients through arterial puncture. Often it is necessary to abandon endovascular intervention in favor of open one. However, our clinic uses an innovative method for removing blood clots using a special Rotarex probe. The probe head rotates at speeds of up to 60,000 revolutions per minute and crushes the clot, after which these fragments are sucked into the probe. This method allows you to remove blood clots without damaging the arteries and solve many problems in endovascular surgery.
Read also: Electrocardiogram sinus rhythm
The main methods of endovascular vascular surgery are angioplasty (expansion of the lumen of the vessel) and stenting - strengthening the vessel wall. After expansion, the artery takes on a normal lumen, but sometimes the dilated vessel, due to its elastic properties, can narrow again. To prevent this from happening, in some cases a special mesh of thin material, called a stent, is left in the lumen. Thanks to angioplasty and stenting, it has become possible to eliminate circulatory disorders in any vascular system, from the vessels of the brain to the arteries of the foot.
Operation technique
The essence of the operation is to insert a long thin catheter into an artery of the heart that is affected by atherosclerosis. The injection site is most often the femoral artery, but sometimes the procedure is performed through arteries that are located in the arms.
Excimer laser is a modern and effective method for treating coronary artery lesions
The entire process is controlled by a radiologist in a special operating room. The X-ray machine on the monitor shows how the catheter is advancing, so you can perform the necessary manipulation in the precisely designated place.
In laser angioplasty, the main instrument is a laser beam. A flexible quartz thread is passed through the bloodstream to the point where there is a cholesterol plaque that is preventing normal blood flow. After this, the laser turns on and begins to affect this plaque using high temperature. Thus, the obstacle gradually disappears and turns into gas. As you can see, laser angioplasty is simple, effective and has minimal recovery time after surgery.
Complications may occur, however, the likelihood is not that high. For example, a catheter can damage an artery and cause bleeding. In addition, there may be swelling and painful bruising in the area where the catheter is inserted, which should disappear after a few days.
In general, this procedure can save you from dangerous complications, so if it is recommended by an experienced specialist, it is best to listen to him. Of course, after it you also need to follow healthy habits and monitor your health.
Articles
Laser conchoplasty
01.11.2014
LASER CONCHOPLASTY
Laser method for destroying hypertrophied ends of the nasal conchae.
When should turbinates be operated on? Surgery is necessary when it is determined that enlarged turbinates are the cause of impaired nasal breathing, chronic rhinitis and inflammation of the paranasal sinuses (chronic sinusitis). Children should be operated on regardless of their age. This is due to the fact that their nasal breathing is more harmful than in adults. They are developmentally delayed and often get sick. Surgery in children has its own characteristics. The turbinates are the cartilaginous projections of the nasal septum. They divide each half of the nasal cavity into nasal passages: upper, middle and lower. Between these shells are the openings of the paranasal sinuses. There are three turbinates, like the nasal passages - upper, middle and lower on each side of the septum. Like the rest of the wall of the nasal cavity, the turbinates are covered with mucous membrane. The presence of turbinates significantly increases the area of the nasal cavity, which contributes to better warming and humidification of the inhaled air. In the mucous membrane of the nasal concha there are special cavities filled with blood. These are cavernous (cavernous) bodies. Blood retention in the corpora cavernosa leads to swelling of the inferior turbinates and increased resistance to air flow, leading to complete blockage of the nasal passages. Blood filling of the cavernous bodies depends on many factors, including the ambient temperature, dustiness of the air, and the presence of inflammation. Blockage of the nasal passages, in turn, leads to blockage of the openings of the paranasal sinuses. Turbinectomy (conchotomy) (Latin concha - conch) is an operation that involves removing the nasal concha.
Methods of surgery for the inferior turbinates Previously, and in some clinics, unfortunately, they still use the Killian method of septal surgery, which has been known since 1904. In this operation, most of the supporting structures of the nasal septum - cartilage and bone - are removed. At the same time, the enlarged turbinates are removed, opening the nasal passages. However, this leads to the absence of the mucous membrane of the nasal septum, and the air is not purified and not warmed to the required extent. A so-called “empty nose” is formed. The first time after the operation, the person is satisfied with the result of the operation. However, over time, crusts begin to appear in the nasal cavity. Over the months, the shape of the nose changes. The anterior part of the septum is retracted, the back of the nose is lowered, and a saddle shape is formed. Because a lot of cartilage and bone are removed from the septum, the septum in some places consists of only two layers of mucosa. Through holes are formed in these places. Crusts dry on them, resulting in bleeding. Due to the change in the shape of the nose, the entrance to the nose becomes narrower. All the changes that occur lead to gradual difficulty in nasal breathing, which is difficult to eliminate.
Modern methods of conchoplasty Currently, laser technology is most often used to remove overgrown cavernous bodies of the turbinates. There are several types of laser surgeries performed for turbinate hypertrophy. This:
| Superficial laser conchoplasty |
| Contact laser conchoplasty |
| Submucosal laser conchoplasty |
The laser method of destroying the hypertrophied ends of the nasal conchae is currently considered the most effective. Such common methods of treating polypous hyperplasia and hypertrophied nasal turbinates, such as removal with a diathermocoagulator, cryodestruction or ultrasonic disintegration, can be accompanied by both bleeding and pronounced edematous reactive processes with microcirculation disorders. In addition, laser technology is also used to treat synechiae (fusions) and nasal atresia, as well as congenital choanal atresia