Burns are a common everyday occurrence. They can also be obtained in production and through careless handling of flammable objects. Typically, such injuries take a long time to heal, are very painful, and cause great discomfort. However, modern techniques can significantly shorten the rehabilitation period and make the recovery period less painful. Laser therapy greatly helps with this.
How does a laser act on the skin: causes of burns
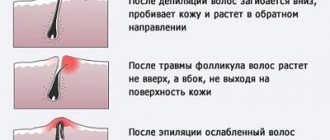
Laser hair removal is the removal of body hair using laser radiation with high energy density. Light exposure to the skin leads to the destruction of follicles and hair root loss. The main causes of thermal burns during the procedure include:
- improper training of a cosmetologist;
- visiting a solarium before the procedure;
- hypersensitivity of the skin;
- laser epilator malfunction.
In 90% of cases, people with dark skin get burns. Due to the increased concentration of melanin, tissues absorb more thermal energy, which provokes thermal injuries.
Selecting the type of laser for your skin type
The choice of laser radiation source depends on the type of skin. To destroy follicles during hair removal, lasers with different wavelengths of light are used:
- neodymium - solid-state emitter with a wavelength of 1060 nm, suitable for people with dark or tanned skin;
- diode – laser emitter with a wavelength of 800 nm, which is suitable for all types of skin;
- alexandrite - a fast-penetrating laser with a wavelength of 700 nm, intended for people with red hair;
- ruby – a laser radiation generator with a working wavelength of 695 nm, which is used to remove light hair from dark skin.
The procedure time depends on the density of the laser beam and the degree of hair growth of the skin.
Depilation should take place in a salon, under the strict guidance of experienced professionals.
The correct choice of light generator prevents unnecessary heating of tissues and damage to the skin.
Signs of a burn after laser hair removal
Burns after laser hair removal look different. The symptomatic picture depends on:
- intensity of light radiation;
- degree of tissue sensitivity;
- duration of laser radiation.
Most often, injuries occur when treating the skin in the bikini area and under the arms. In these areas, the protective layer of the epidermis is thin, making it vulnerable to heat damage. A burn from laser hair removal is indicated by:
- redness;
- swelling;
- itching;
- burning;
- peeling;
- blisters;
- crusts in the lesion.
In 80% of cases, after hardware hair removal, shallow burns of 1st and 2nd degrees are obtained. First, the tissues swell and acquire a reddish tint. When the keratinized epithelium and basal layer of the dermis are damaged, bubbles with transparent contents form. Since the sensory receptors remain unaffected, patients complain of burning or pain.
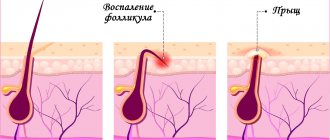
Improper first aid increases the risk of infectious inflammation. When pyogenic bacteria penetrate the wound, the condition of the tissue worsens. Ulcers form, from which a light green or yellow exudate with a putrefactive odor is released. Infectious inflammation prevents scarring of the skin and provokes complications in the form of trophic ulcers and fistulas.
First aid
A burn after laser hair removal requires immediate treatment of the damaged tissue. First aid involves the following measures:
- Cooling. To stop the heat exposure and prevent further destruction of soft tissue, you need to place the affected area under running water for 10-15 minutes. Alternatives include an ice bag, cold compress, and hypothermic pack. But you should not use them for more than 10 minutes to avoid frostbite.
- Anesthesia. In case of severe pain, the victim is given non-narcotic analgesics - Piroxicam, Ketoprofen, Amidopyrine. To enhance their effect, take 1-2 Spazmalgon tablets.
- Treatment with anti-burn agents. The area of redness is lubricated with ointments with anti-inflammatory and antiseptic effects - Rescuer, Furacilin, Sintomycin. If the epidermis is hypersensitive to drugs, the skin is treated with Panthenol or Dexpanthenol spray. The foam is evenly applied to the affected area, covering 2 cm of healthy tissue around the burn.
- Applying a bandage. Blistering rashes on the burned area are covered with a sterile bandage. The skin is pre-treated with antiseptic ointments - Betadine, Dioxidin, Miramistin, etc. They prevent the penetration of infection and the transformation of the transparent exudate of the vesicles into pus.
If you are burned by laser radiation, you should not treat the affected areas with folk remedies - egg whites with flour, alcohol tinctures, badger fat, vegetable oils, etc. Self-medication is fraught with an increase in the area of the burn and infectious complications. For superficial burns, further treatment is continued at home.
Medicinal plants
In folk medicine, compresses from certain plants are used to avoid a burn scar:
- onion - an extract from this plant dissolves fibrin (a component of insoluble protein that creates blood clots), and therefore smoothes and lightens the scar. Onions also have antibacterial properties;
- flax seeds, and specifically the oils they contain, have an anti-inflammatory effect, and also soften and facilitate wound healing and prevent the occurrence of visible scars;
- calendula officinalis - flower extracts of this plant (oil and alcoholic) accelerate the healing process of all types of wounds, including burn scars;
- Rose seed oil makes the skin elastic and reduces the appearance of scars.
Treatment and skin care after a burn
For relatively shallow burns, only local therapy with antiseptic, analgesic, and wound-healing drugs is carried out. The duration of treatment varies from 3 to 14 days.
If the skin is damaged along with a mole after hair removal, you should consult a doctor to rule out malignancy.
At the initial stage, the following ointments and gels are used:
- Amprovisol is an analgesic and anti-inflammatory drug that has a cooling effect. Prescribed for thermal burns of 1st and 2nd degree. The aerosol is sprayed onto cleansed skin 1-3 times a day.
- Argakol is a gel with glycerol and dioxidine, which has a disinfecting, analgesic and wound-healing effect. Prevents the formation of blisters, protects burn wounds from infections. Apply a thin layer to laser burns 2-3 times a day.
- Dettol Benzalkonium Chloride is a disinfectant solution with anti-inflammatory properties. Intended for the treatment of laser burns complicated by purulent inflammation. The wound is washed 2-4 times a day for a week.
Treatment of laser burns at home is carried out with wound healing ointments. They are used after opening the vesicles to quickly restore the integrity of the epidermis. The most effective pharmaceutical products include:
- Lioxazine is a napkin made of non-woven material with hydrogel impregnation. It has a bactericidal and regenerating effect on burned tissues. Apply to damaged tissues for 30 minutes up to 3 times a day.
- Dexpanthenol is a wound-healing ointment with provitamin B5, which accelerates metabolism in the skin. Accelerates the healing of burns, stimulates local immunity.
- Aekol is a vitamin solution that exhibits antioxidant, wound healing and anti-inflammatory effects. Heals thermal burns and trophic ulcers after laser exposure.
- Algofin is an antimicrobial ointment with a wound-healing effect. Used in combination therapy of burns caused by laser and radiation.
To treat bacterial inflammation of the skin and prevent purulent complications, drugs with antimicrobial action are prescribed:
- Altargo is an antibacterial ointment that prevents purulent inflammation of burns. Apply to damaged areas twice a day for 5 days.
- Dioxidin is a broad-spectrum antibiotic intended for the prevention and treatment of purulent complications. The ointment is used to treat burns once a day for 2 weeks.
- Silvederm is an antimicrobial ointment that accelerates the healing of 1st and 2nd degree burn wounds. Apply to cleansed skin under a bandage 2 times a day.
There are many sebaceous and sweat glands concentrated in the armpits and groin area. Therefore, burns in these areas are often accompanied by infectious inflammation. For abscesses and abscesses, patients are prescribed systemic antibacterial therapy with drugs from the group of cephalosporins, fluoroquinolones - Ceftriaxone, Cefazolin, Pefloxacin.
The main stages of the laser scar resurfacing procedure
- Consultation . After collecting your medical history, the doctor will discuss with you the required number of sessions and name the price for scar removal. If the doctor has doubts, you will be prescribed laboratory diagnostics to rule out the presence of contraindications. The doctor may suggest other ways to solve the problem if the laser method is not recommended for you.
- Preparatory stage . The skin is cleaned and an anesthetic cream is applied if necessary.
- Setting the depth, frequency and power of the laser pulse, selecting the appropriate program.
- One test pulse . Conducted to determine the effectiveness of the selected settings.
- The procedure itself . Its duration on average ranges from 5 minutes to half an hour, depending on the area of scar tissue. The session is quite comfortable.
- Treating the skin with an antiseptic and anti-inflammatory agent.
- Receive recommendations for home care . The doctor will help you choose medications and care products. To speed up regeneration, dietary supplements can be prescribed.
What not to do after the procedure
After hair removal, you need to follow the rules for caring for damaged skin. Ignoring them often causes injuries and complications.
In most cases, cosmetologists advise women to use special restorative creams after laser hair removal.
To avoid unpleasant consequences, you should:
- avoid getting the skin wet for 24 hours after laser treatment;
- stop using hard washcloths for three days;
- avoid exposure to sunlight on the skin;
- refrain from visiting swimming pools and saunas for 1.5-2 weeks;
- Avoid visiting solariums for 14 days.
When removing hair from the facial area, it is not recommended to use scrubs, resort to chemical peeling, or apply self-tanning cream for 10-14 days. You should also refrain from excessive physical activity. For people with excessive skin pigmentation, sunbathing and body massage are contraindicated for a month. Failure to follow the recommendations can result in irritation and superficial burns.
Typically, a laser hair removal course consists of 3-8 sessions. During this period, you need to use regenerating ointments, moisturizing and cooling creams. They restore the hydrolipid mantle of the epidermis. Thanks to this, the skin becomes less sensitive to the effects of laser radiation.
Treatment at home
You can take care of damaged skin areas at home, but do this only using safe methods. Within 5 days after receiving a burn, you need to treat the area with Panthenol ointment. Apply the ointment carefully until completely absorbed 2 times a day. After application, you need to wait 20-25 minutes until it is completely absorbed.
After the burn goes away, the skin in this area will be dry; it needs to be nourished and moisturized with special creams. This must be done until it recovers again; elastic and soft skin without peeling can be considered an improvement.
But creams should be moisturizing, and not greasy, which can create a film on the damaged area, interfering with its healing and oxygenation. Therefore, oils and lotions for moisturizing the skin after a burn are prohibited.
- Blisters, if they form, cannot be punctured, as they will heal more slowly and can provoke tissue infection.
- Treatment of burns must be gradual and correct, so that after healing there are no scars left on the skin.
Possible complications
Laser hair removal devices rarely cause negative consequences. But when depilating the bikini, armpits, groin and other areas with sensitive skin, the following sometimes occur:
- redness;
- perifollicular edema;
- hyperpigmentation;
- photosensitivity;
- folliculitis;
- exacerbation of herpes.
The severity of side effects depends on the density of the laser beam, hair and skin color. Complications are more common in dark-skinned people, since darker skin absorbs more thermal energy. Because of this, not only the hair follicles are destroyed, but also the surrounding tissues.
Who is contraindicated for laser hair removal?
Laser hair removal on the body has absolute and relative contraindications. The first category includes:
- decompensated diabetes mellitus;
- squamous cell skin cancer;
- blonde hair;
- low blood clotting;
- leukemia;
- individual intolerance to the procedure.
The procedure is not performed on persons under 18 years of age. Relative contraindications include:
- exacerbation of herpes;
- hypopigmentation;
- fresh tan;
- relapses of allergic dermatosis;
- burns, acne, pimples in the treated area;
- pregnancy;
- multiple moles on the body;
- phlebeurysm.
Ignoring contraindications is fraught with burns, keloid scars, and malignancy of tumors. In patients with excessive sweating and sebum secretion, the risk of inflammation of the hair follicles increases. Folliculitis in people with immunodeficiency is dangerous due to furunculosis.
If you have dark skin, you should not use alexandrite lasers, as they are highly likely to cause deep burns. You should also refrain from hair removal during exacerbation of ENT diseases - laryngitis, bronchitis, sinusitis, etc.
Cost of laser scar resurfacing procedure
The price for laser scar resurfacing in Moscow at the Marina Ryabus clinic ranges from 300 to 600 rubles. for 1 sq.cm. The service is provided after an examination and consultation with a doctor, so you will know in advance the exact cost of scar removal.
| Procedure | Price | |
| Treatment of scar tissue 1 cm² Fotona using ND:YAG laser | 300,00 | Sign up |
| Fractional laser treatment of scars and stretch marks 1 cm² Fotona | 600,00 | Sign up |
| Postpartum recovery with fractional treatment of scar tissue (after perineotomy and episiotomy) Fotona | 25 000,00 | Sign up |
| Fractional treatment of scar tissue in aesthetic gynecology up to 10 cm² Fotona | 5 000,00 | Sign up |
There are also injection methods for scar removal. In our clinic, two drugs are used for this - Kenalog and Diprospan:
How the scars will be removed is determined by the doctor during the consultation. Marina Ryabus Clinic always offers you only the most effective procedures in your case.
While you are undergoing scar treatment, consider other services. We offer to rejuvenate the skin using Liftera and Fotona devices, and shape the figure using Ulfit and Velashape. We also have advanced injection techniques in our arsenal: volumization and restoration of facial geometry using Radiesse, Juvederm, Belotero. And, of course, biorevitalization, mesotherapy, peelings, ultrasound cleaning, etc. are at your service. At Marina Ryabus’s clinic, you will see an endocrinologist-gynecologist who will help you eliminate deficiencies and improve your well-being.
To make an appointment for a consultation, call: +7 (499) 397-71-30; or leave a request in the feedback form.
Prevention of skin trauma
To avoid burns, you need to follow the rules for preparing the skin for the laser procedure:
- 3-4 days before hair removal, do not use alcohol-containing solutions or ointments;
- do not visit solariums or tan in the sun for 14 days;
- do not remove hair by other means within 20 days;
- do not take tetracycline antibiotics 2 weeks before the procedure.
To achieve the desired effect, it is recommended to shave the epilation area 8 hours before the session. After each procedure, you need to use cooling gels that prevent overheating of the skin and superficial burns. Compliance with the recommendations prevents side effects and complications.
MATRIX, LASMIK
Professor L.I. Gerasimova, Burn Center of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky
Burns have a long history, however, the methods, means and tactics of treating burned victims are changing as knowledge in the field of burn pathology and scientific and technological progress increase. The relevance of the problem of burns in modern medicine is determined by the frequency of their occurrence in everyday life and at work, in the context of increasingly frequent military conflicts, terrorist attacks, man-made disasters and natural disasters. According to the World Health Organization and publications of many authors, burns occupy 2-8 place among other injuries, reaching 380 cases in Russia, 290-300 cases per 100,000 population in the USA and Japan, which determines the social and medical significance of the problem.
In acute burn pathology, long periods of hospitalization remain, a significant number of infectious and other complications, and high mortality (32-82%) among severely burned people and elderly and senile people. All this dictates the need for further improvement of existing and still new approaches that can increase the effectiveness and results of traditional methods of treating burnt patients.
One of these approaches was the use of laser (LT) and magnetic laser therapy (MLT) in more than 2500 victims with acute burn injury who were admitted to the burn center of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky from 1980 to 2003 The development of this area was carried out in collaboration with other clinical and laboratory divisions of the institute and a number of industrial enterprises and firms involved in the production and creation of medical laser equipment, including. Over the years, we have been involved in the testing and use of 18 different types of medical lasers. In our work, we used lasers operating in the ultraviolet (UV), visible red (VR) and infrared (IR) ranges of the optical spectrum. Local irradiation of burn wounds and skin grafts was carried out, through skin exposure to reflexogenic zones and biologically active points (BAP), intravenous laser blood irradiation (BLOCK), and endobronchial exposure. The accumulated experience has allowed us. make proposals for operating instructions for a number of devices and develop new technologies, strategy, tactics and methodological recommendations for the use of radiation therapy. and MLT for patients with burns of varying severity and location.
Despite the fact that the mechanism of action of LT and MLT on the body of patients has not been fully deciphered, the results of our own research and literature data give reason to believe that their use has a complex and diverse effect, manifested in the systemic, organ, tissue, cellular, molecular and submolecular levels. Without going into a discussion of individual aspects of the mechanism of action of LT and MLT, we note that in clinical settings their main manifestation is an anti-inflammatory, analgesic, immunomodulatory effect and stimulation of reparative processes.
In the complex treatment of burn patients, we widely used laser radiation in the VC range of the spectrum, starting its use in 1984 with a large-sized helium-neon laser physiotherapeutic unit LT-1 with a wavelength of 632 nm and a radiation power of 12 mW, and then a 20 mW unit ULF-01 “Berry”. We used these first generation lasers to treat superficial burns of P-SHA degree. The research results showed that VC laser radiation is well tolerated by patients and does not cause any adverse reactions or complications at a single dose of 380-508 mJ/cm2 on a wound with an area of 1% of the body surface (160 cm2). Against the background of laser therapy, inflammation in the tissues significantly decreased, the growth of the marginal epithelium increased, and after 4-5 sessions epithelization of second-degree burns occurred. In case of SA grade burns, the wounds healed completely after 5-7 sessions. The overall effect of VC laser therapy was expressed in improving the quality of treatment, reducing the consumption of medications and the length of hospitalization for patients with second-degree burns by 3-4 days, for patients with third-degree burns by 5-7 days.
For deep burns of IV-IV degree, VC laser radiation was used in the pre-, intra- and post-operative periods. A course of treatment of 3-5 sessions ensured the formation of a complete granulation cover. During the operation, the subdermal surface of the skin graft removed by the dermatome was irradiated at a dose of 200-250 mJ/cm2. The total area of the irradiated skin grafts, as a rule, did not exceed 2400 cm2 (15% of the body surface). In the postoperative period, VC laser irradiation was used on residual wounds at the junction of the grafted skin and on mesh skin flaps. The developed treatment tactics increased the effectiveness of surgical treatment of deep burns by 10%, reduced the length of hospitalization of patients and the economic costs of their care and medications by 3.7 days compared to traditional methods.
Currently, to replace these large-sized lasers, we have successfully used a new miniature ALT “Kreolka”, developed at the Tekhnika-Pro company (Moscow), with a wavelength of 635 nm, operating in a continuous mode, having a power of 5 mW and a magnetic attachment in 25 mts. The light weight of the “Creole” (50 g) and its shape create optimal convenience for intraoperative irradiation of the subdermal surface of skin grafts during transplantation in patients with deep burns. I believe that the use of ALT “Creolka” has great prospects for growing cultured fibroblasts and keratinocytes, the use of which in the treatment of extensive burns is widely studied both abroad and in our country.
A great achievement in the treatment of patients with extensive burns was ILBI, which we have been using in the VC range of the optical spectrum since 1980. In our work for many years, we used the ALT-01 GNL with a wavelength of 632 nm, using a power output of the light guide of 1.5-2 .0 mW and irradiation time 900-1200 s. Quantum hemotherapy sessions were carried out daily for 3-5 days in a row during the period of acute burn toxemia in 65 patients with III-IV degree burns on an area of 25-50% of the body surface, where the proportion of deep lesions was 20-45%. The causes of burns were flames and boiling water. Indications for VC ILBI included severe intoxication that occurred after removing patients from a state of burn shock, the need to relieve congestive venous congestion in the lungs, and the prevention of pneumonia. The control group consisted of 52 patients comparable in age and burn severity. The effect of VC ILBI is manifested in a significant improvement in the well-being of patients, a decrease in tissue swelling and pain, normalization of sleep, and an increase in appetite. Elimination of stagnation in the pulmonary circulation, according to clinical, radiological and laboratory studies, indicated an improvement in microcirculation processes and correlated with a significant decrease in the initially high content of serotonin in the blood plasma immediately after the first session of VC BLOCK, indicating an improvement in its metabolism, occurring mainly in lung tissue. The use of VC ILBI contributed to the prevention of the development of pneumonia. If pneumonia did occur during periods of shock or toxemia, intravenous ILBI allowed it to be stopped in 5-8 days versus 12-15 days in the control group, and the preventive effect for this severe complication of burn disease in the risk group reached 76%. The use of VC ILBI had a positive effect on peripheral blood parameters, eliminated red blood cell edema, and stopped lymphopenia, 4-5 days ahead of the improvement in these parameters with traditional treatment.
The appearance of the semiconductor ALT “Mulat” (radiation wavelength 630 nm) attracted our attention due to its design features: small dimensions and weight, the presence of a radiation power meter and timer, a main one and attached disposable light guides with needles that allow puncturing peripheral veins of small diameter, which is essential facilitates the procedure itself. ALT “Mulatto” allowed us to expand the indications for the use of VC ILBI not only for extensive, but also for frequently occurring limited-area thermal injury of the distal extremities (hands, feet), in order to avoid deepening of burns due to tissue edema, progression of ischemia, hypoxia and create optimal conditions for their healing. In recent years, we have successfully used ALT “Mulat” in more than 250 patients with superficial burns and deep burns in the pre- and postoperative periods. The use of ILBI ensured 96-100% engraftment of autoskin and reduced the restoration of epithelial cover in the cells of mesh grafts to 4-6 days when using an expansion ratio of their area of 1:3. The results of the research allowed us in 1999 to develop a guide for the use of ALT “Mulat” for thermal injury, published by the Tekhnika company.
The creation of semiconductor lasers generating IR radiation with a wavelength of 820-890 nm was the latest achievement of quantum electronics, thanks to which these lasers have become widely used in the treatment of acute and chronic degenerative-dystrophic and inflammatory diseases. The high penetrating ability of IR laser radiation has made it possible to influence on organs and tissues located at a depth of 3-4 cm, and the attachment of magnetic attachments to the laser emitter increased the penetration depth to 6-8 cm. Thus, two new methods appeared in the arsenal of LT means: IR LT and IR ST. The combined effect of IR MLT has led to qualitatively new biophysical processes and phenomena in tissues, significantly increasing the therapeutic effect in diseases of inflammatory etiology and traumatic injuries, including burns.
The first in world practice to carry out IR MLT was the “Pattern” laser on gallium arsenide, developed by A.R. Evstigneev in Kaluga, with subsequent equipment of the laser with magnetic attachments. It is from this device that I study the effectiveness and development of the IR MLT method in relation to the treatment of burnt patients, including in cases of group and mass admissions to the Moscow Burn Center from sites of man-made disasters and natural disasters.
Local application of IR MLT lasers “Uzor”, “Lazur”, “Erga”, “Loomis”, “ALTO-05”, “Mutang”, “Milta-F”, etc. has proven itself in the treatment of more than 950 patients with burns . The radiation doses we developed for a wound with an area of 1% of the body surface were, in the minimum version, 60-80 mJ/cm2, in the maximum - 120-160 mJ/cm2, magnetic field induction - 30-100 mTs. MLT began from the first days of admission of burnt patients to the center, daily, 5-10 sessions per course of treatment. MLT was performed on an open wound during dressings, and outside them through a bandage. MLT was also used 2-3 days before skin transplant surgery, and after it according to indications, but not more than 5 sessions. Such treatment, as a rule, ensured a smooth course of the wound process, rapid relief of edema, improvement of microcirculation, and indicators of local and general homeostasis. With surgical treatment, the engraftment of skin grafts increased to 96-100%, versus 85-90% in the control. The consumption of medications was significantly reduced, and the length of hospitalization was reduced by 4-5 days. For the prevention and treatment of pneumonia, MLT was performed along the transverse vertebrae of the thoracic spine, and a laser beam was scanned from the front along the intercostal spaces. The power density was 5-10 mW/cm2, the exposure was 8 s per point with the wound closed with a bandage and 4 s with an open wound. The total number of points is no more than 60, single radiation dose is 1.8-4.8 J/cm2. The course of treatment for the prevention of pneumonia is 5 sessions, if it is present - 5-8 sessions. The preventive effect of this method in the risk group was 80%, the time for relief of pneumonia was halved compared to patients who did not receive MLT.
In recent years, I have developed new technologies for the complex use of laser therapy with such original physical-energetic methods as mesodiencephalic modulation (MDM), aeroion therapy (AIT) and ozone therapy (OT), which have made it possible to increase the effectiveness of treatment of burnt patients. Center staff involved in the treatment of patients and the introduction of these new technologies, Gerasimova L.I., Artemova V.V., Shakhlamov M.V., Loginov L.P., Spiridonova T.G., Smirnov S.V., Dondrikova E.S., Sokolova T.A. in 1998 they were awarded the title of Laureate of the Moscow City Hall Prize. In 1995, Doctor of Medical Sciences, Professor Gerasimova L.I. was elected academician of the Laser Academy of Sciences of the Russian Federation, and in 2000 she became a laureate of the Prize named after. A.L. Chizhevsky.
Thus, an analysis of the research results showed that the clinical effectiveness of treatment in patients treated with RT and MLT is significantly higher than in patients treated only with traditional methods. The high preventive and therapeutic value of these methods, which are practically harmless, the most physiological and economically beneficial, has been established. The use of new technologies for the integrated use of LT and MLT with the methods of MDM, AIT and OT can further improve the quality and overall effectiveness of treatment for burnt victims. Our data have been repeatedly included in the programs of seminars, symposia, conferences and congresses dedicated to the problem of burns and laser medicine. All this allows us to once again recommend the use of these methods in the practice of specialized burn centers and departments, and the developed methods may be of interest to surgeons, traumatologists, resuscitators and a wide range of doctors involved in laser therapy, as well as specialist developers of modern medical laser equipment.
article published in the newspaper “Lazer=Express”, No. 5, 2003