Aging is a multi-stage and multi-factor process. A person’s face does not change in just one decade, and not only changes at the skin level reflect the fading of our face. Everything changes, from bone structures and ligaments to fat packets. Superficial and deep fatty compartments provide support for overlying tissues and create volume. Changes in the area of these anatomical formations have a particularly strong impact on the face. On estet-portal.com, read what superficial fat packets exist, where they are located, and how to correctly correct them.
- Facial anatomy: location of superficial fat packets
- Aging processes of superficial fat packets
- Features of correction of superficial fatty tissues
Facial anatomy: location of superficial fat packets
Infraorbital fat (IF) Its upper edge corresponds to the lacrimal groove and the palpebromalar groove. The upper limit of this package is the orbicular suspensory ligament (ORL) , which originates 1–2 mm below the bony edge of the orbit and passes through the orbicularis oculi muscle to reach the dermis. This ligament starts from the periosteum below the bony edge of the orbit and goes to the fascia lining the inner surface of the orbicularis oculi muscle. ORL contributes to the formation of the tear trough and palpebromalar groove . Situated cephalad to these two sulci, the orbicularis oculi muscle lies immediately beneath the skin of the lower eyelid, its caudal portion covered by infraorbital fat. The lower border of the infraorbital fat pad is the zygomatic ligament. This fat packet has a high tendency to retain water , which often causes the formation of the so-called. malar edema.
Superficial medial cheek fat (SMCF) is triangular in shape and is located between the infraorbital and nasolabial fat pads, caudal to the infraorbital fat pad, from which it is separated by the zygomatic ligament. The lateral borders of this fat pad are the zygomaticus major muscle and the middle buccal fat pad. Below and medial to the superficial medial buccal fat pad is the nasolabial fat pad, located parallel to the nasolabial fold.
Nasolabial fat (NLF ) has an oblong shape, located lateral to the nasal pyramid, parallel and cranial to the nasolabial fold. The ORL forms the upper boundary of this fat pad. It borders superolaterally with the superficial medial buccal fat pad, and the middle buccal septum (or buccomaxillary ligament) separates these two fat pads. Inferomedially it borders the nasolabial fold. Its lower part borders on the maxillary fat pad and overlaps it.
Middle cheek fat (MCF) Located lateral to the medial buccal fat pad, its upper border is the zygomaticocutaneous ligament. Above this packet the ligament is thick and forms McGregor's point . The middle buccal fat pad does not extend above the lower edge of the zygomatic arch. Anteriorly it is bordered by the masseteric ligament, which begins below McGregor's point and descends vertically down along the anterior border of the masseter muscle. This ligament originates from the fascia of the masseter muscle and is intertwined with the SMAS and the overlying dermis of the buccal region. The middle buccal fat pad borders laterally on the lateral temporobuccal fat pad and is separated from it by the lateral buccal septum (or parotid masticatory septum). Caudal to the middle buccal fat pad is the maxillary fat pad.
Lateral temporal-cheek fat (LTCF) This is the most lateral fat pad of the cheek, it is in direct contact with the parotid gland and connects the temporal fat pad with the cervical subcutaneous fat. The buccal part is tightly adjacent to the fascia of the parotid gland.
Superior jaw fat (SJF) Located below the nasolabial fat. Its lateral border is the middle buccal fat pad.
Inferior jaw fat (IJF) is located lower in relation to the middle buccal and upper jaw fat. Its medial border is the mandibular ligament, and its posterior border is the lateral temporobuccal fat pad. The lower border is formed by the mandibular septa.
The first three superficial fat pads (infraorbital fat pad, medial buccal fat pad, and nasolabial fat pad) are described as a unique anatomical structure: the malar fat pad . It has a triangular shape with a base parallel to the nasolabial fold, with the apex in the region of the highest part of the malar zone.
The malar fat pad is loosely adherent to the SMAS, but tightly adherent to the skin. At a young age, it is supported by numerous fibroelastic fascial septa that run through the entire mass of buccal fat and originate from the underlying superficial fascia that attaches the facial muscles to the skin.
Read the most current articles in Telegram !
How was the FaceRecurve® concept invented?
Dr. LeLouarn has spent a long time studying the effects of aging on the periorbital area of his patients and, in particular, those manifestations that form “dips” around the eyes.
He could not explain to himself how gravity could become “responsible” for the severity of these depressions with age, because these grooves are formed not on the surface, but at a deeper level, and “fall” even deeper into the bone over time. The skin tissues, logically, should sag vertically, descending (toward the mouth), especially taking into account the fact that there are no anatomically determined fixation points in this area. There is such a story. One day an officer told a young sergeant who was trying unsuccessfully to understand why a certain hill that was clearly indicated on the map was not there: “If reality does not match the map, then the map is drawn incorrectly.” In the case of structural aging, it seems especially appropriate to revise the generally accepted (and many times described) theory. Dr. LeLouarne's work in the field of dynamic anatomy on the "aging gaze" led him to the discovery that contraction of a certain segment of the zygomatic part of the orbicularis oculi muscle and, more specifically, its upper part, may cause the appearance of those notorious rings under the eyes. He noticed that each time this muscle segment contracts, as in the forced blink reflex, it becomes a fulcrum on the edge of the orbital bone. It is possible that, repeated a thousand times, the contraction of this segment will, over time, lead to a rise of fatty tissue between this muscle and the bone, which will consequently create bags under the eyes, as well as eye bags, thereby forming rings around the eyes, visible even in a state of peace (here the expression “like between a rock and a hard place” will be more relevant than ever).
PHOTO 11
. When contracting, the eye muscles (orbicularisoculi) press on the orbit. More broadly, by looking at the face as a whole, surgeons and anatomists have long been able to observe structural differences between the face of a young and an old person. On young faces, deep-lying portions of fat are found in large quantities, “conglomerates”, located deep in the muscles, while superficial fat, located between the skin and muscle, forms a uniform layer under the skin.
PHOTO 12
. Deep fat on the face of a young (left) and elderly person (right). On the faces of more mature people, one can observe the process of thinning of deep adipose tissue and, on the contrary, an increase in the volume of subcutaneous fat, the latter being unevenly distributed. Then we can assume that the contraction of the facial muscles repeated a million times in facial expressions can provoke a displacement or decrease in the volume of adipose tissue, which will gradually lead to a more noticeable “immersion” of the tissues in the orbital area and the formation of deep furrows at rest with the above-mentioned development of excess volumes.
In addition, the use of botulinum toxin in cosmetic procedures has led Dr. LeLouarne to believe that the muscles involved in expressive facial expressions may contract over time (which is radically different from the widely held belief that they should instead relax and stretch as and skin, under the influence of gravity). Simply put, for example, if you can smooth out wrinkles and crow's feet and relax muscles by injecting them with a certain amount of botulinum toxin, this means that aging causes muscles to "retract" or decrease their length.
PHOTO 13
. Crow's feet at rest at 35/40 years. The result obtained with botulinum toxin injection is relaxation of the muscle in order to smooth out crow's feet. You should also pay attention to the rise of the eyebrow tail.
Therefore, in order for young muscles, when contracting, to reduce the volume of deep fat bags and increase the volume of the superficial fat mass that creates the bags, they must be convex and long at rest and flat and short when contracting. As we age, muscles are forced to contract on their own, causing them to lose their convexity (i.e., remain in a compressed state). This may be the only logical explanation for the displacement of adipose tissue during articulation.
And if this theory is true, it could be tested:
- Radiological examination would have to confirm muscle contraction and loss of convexity with age (or contraction);
- Moreover, the theory would have to prove the same thing during anatomical dissection;
- Last but not least, this would have to be clinically applicable in the treatment of structural aging and therefore enable the introduction of new technical techniques to improve the effectiveness of treatment.
Radiologist Didier Buthiau
from the Institute of Radiology in Paris conducted an MRI study of the effects and constants that could provide evidence of muscle “curvature”.
This was the moment of truth, confirming the correctness of the theory. Dr. Buteau made a series of films, and then asked a surgeon he knew to tell, based only on the image of the muscles, whether they belonged to a young or an old person. All that was available to the surgeon was the muscle bends and the distribution of the deep and superficial layers of adipose tissue. The surgeon's answers completely confirmed the theory! In young subjects, at rest, the muscles curved convexly, resting on the fat compartment lying in the depths. Over time, the muscles became straighter and shorter, while the deep fat became thinner and the surface fat increased in volume.
PHOTO14
. MRI performed by Dr. Buteau, Institute of Radiology, Paris.
The multistep mechanism involved in the structural aging process can be further studied in more detail. Models of muscle flattening and fat removal muscle are the theoretical basis of the concept of FaceRecurve®.
Aging processes of superficial fat packets
The aging process causes hypertrophy of the volume of the superficial medial buccal fat pad with slight ptosis of its lower part . Volume increases in the lower two-thirds and remains stable in the upper third.
Nasolabial fat pad (NLF). There is a slight shift in the volume of adipose tissue. In older patients, the sagittal diameter of the upper third becomes smaller, and the sagittal diameter of the lower third increases. These changes create a general hypertrophy of the lower part of the malar fat pad due to ptosis and caudal migration of fat tissue.
Aging of the malar fat pad can be described as ptotic/hypertrophic, resulting in an increase in the depth of the nasolabial fold.
Middle buccal fat (MCF). Like the malar fat pad, it is weakly attached to the SMAS plane, and its aging process is characterized by ptosis, caudal migration of fat and hypertrophy. These changes result in an increase in the convexity of the central part of the cheek .
Lateral temporobuccal fat pad (LTCF) . Tightly attached to the parotid fascia without any deep fat pad between them. Aging is determined by hypotrophic involution and usually does not tend to migrate caudally.
Facial anatomy for cosmetologists: how to avoid dangerous areas
Features of aging
The condition and appearance of the skin depends not only on nature or on the work of the master. Facial aging itself is a combination of biochemical, physiological and histological changes occurring in the skin.
It is important to understand the mechanism of skin changes because there are different types of aging. They contain exactly those reasons that can be influenced and preserve the youth of the face, since each type requires its own approach.
In total, there are 6 types of age-related changes; let’s look at them in more detail.
Anatomy of the glabellar area: glabellar complex, main arteries
The glabellar complex of muscles in the area between the eyebrows consists of:
- muscles of the proud (procerus);
- muscle that wrinkles the eyebrow (corrugator supercilii);
- muscle that lowers the eyebrow (depressor supercilii).
The corrugator brow originates from the medial part of the brow ridge on the frontal bone and enters the skin of the middle part of the eyebrow. The supratrochlear neurovascular bundle exits through the corrugator supercilii and provides sensation and blood supply to the central part of the forehead. The corrugator muscle compresses the medial portion of the eyebrow.
In 2012, Pessa and Rohrich found that adipose tissue compartments in the glabellar complex lead to the appearance of vertical lines (folds). The cosmetologist can use these folds as indicators of the position of the supratrochlear artery and nerve . When the glabellar complex contracts, three folds :
- median;
- corrugatory;
- supraorbital.
Between them there are fat compartments – medial and lateral. The location of the supratrochlear artery is indicated by the corrugator, and the location of the supraorbital artery by the supraorbital fold, respectively.
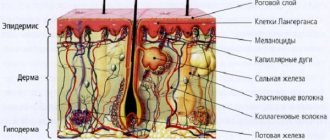
Layers of skin
The skin has several functions, each of which is performed by a specific type of cell and its associated blood and lymphatic vessels. The more active the processes of exchange, nutrition and respiration occur inside the cell, the more aesthetically pleasing the face and body look. A thorough study of the structure of facial skin by biologists and cosmetologists is carried out in order to identify the causes and find means to prolong youth and beauty. What does it consist of?
The structure of the epidermis
The epidermis is the top layer of skin that performs a protective function. Its thickness, depending on age and physiology, reaches 0.5-1.5 mm; it consists of five layers:
- basal;
- spiny;
- grainy;
- brilliant;
- horny.
Basal is the lowest layer in which the embryos of new cells form and rise to the upper layers. The renewal and regeneration of the epidermis depends on the condition and work of the cells of this layer.
The horny layer is the top layer, represented by dead cells - scales, which self-remove over time or are removed using scrubs.
The stratum spinosum received its name due to its spine-like structure, which are located in the epidermis in several rows (from 5 to 10).
The granular layer is 4-5 rows of keratinocytes involved in protein synthesis and maintaining water balance.
The shiny layer is formed by flat cells that merge into a light-refracting mass and are responsible for the strength and elasticity of the skin.
Between these layers of cells there is a jelly-like liquid that retains moisture inside the cells, prevents it from evaporating and does not allow foreign bodies to pass through.
Structure of the dermis
Deeper than the epidermis is the dermis. Consists of two layers: papillary and reticular. They are penetrated by blood and lymphatic vessels and glands. The reticular row of cells contains hair follicles and nerve endings. But of particular interest from a cosmetological point of view are collagen and elastane fibers, which give the skin elasticity and continuity.
Through the network of capillaries of the dermis, the upper layer receives nutrition and oxygen. With age, capillaries lose their integrity and partially cease to perform their functions. As a result, the upper layer - the epidermis - does not receive enough nutrients and oxygen, becomes thinner and becomes wrinkled.
The dermis contains components - fibroblasts, which destroy damaged structures and reproduce new ones. This applies to collagen fibers and hyaluronic acid. Young skin has active fibroblasts, old skin has passive ones, so the formation of collagen in it is slowed down. The dermis is dotted with blood vessels, which, in addition to nutrition, give the face a pink tint.
The structure of the hypodermis
This is a series of fat cells penetrated by capillaries and nerve fibers, as well as a layer of connective tissue. In this layer, nutrients and vitamins accumulate, which later enter the dermis and epidermis. Rapid fading of the skin and dull color indicate depletion of nutrient reserves. From a cosmetological point of view, this problem is easy to solve. It is enough to use deep penetration masks and serums with a high concentration of amino acids, vitamins and other components.
What determines the condition and color of the skin?
Elasticity, freshness, color and other characteristics of the face depend on the structure and condition of all layers. So the pigment melanin, which responds to dark color and tan, is formed and accumulates in the epidermis. There are also pores here that bring sweat, impurities and toxins to the surface.
The intercellular fluid in the upper rows of cells is represented by ceramides, cholesterol and fatty acids, which are responsible for skin type. Thus, the predominance of fatty acids and cholesterol makes the surface of the face oily, and a low concentration of ceramides makes it dry and flaky. The correct balance of intercellular fluid components makes the face beautiful and elastic. This balance can be achieved with the help of special creams and serums, as well as cosmetic procedures.
Tone and elasticity are provided by collagen fibers and hyaluronic acid located in the dermis. It has a whole network of collagen, the integrity and elasticity of which is responsible for youth. Hyaluronic acid is a polysaccharide that fills the space between collagen fibers. Its main task is to bind liquid and prevent evaporation. After the discovery of this substance, cosmetic brands began to include it in anti-aging and moisturizing face and body care products.
A competent cosmetologist, knowing the structure of facial skin, can determine in which layer the problem is localized and what needs to be done to eliminate it. But individual characteristics are also important here. Some people, due to hereditary factors, have thin and pale skin, others have rough and dense skin, and others are prone to oiliness and acne. Cosmetology is a science that still has a lot to discover, and the starting point is the structure of the skin.
Vascular and nervous tissue of the face
Facial anatomy necessarily teaches the location of the vascular network on the human face - small venous ducts that supply facial tissue with important nutrients. For cosmetologists, the problem of blood vessels, or rosacea, is the most common complaint for which women turn to aesthetic medicine for help.
Cuperosis is a genetic predisposition of almost every person to the appearance of redness and unevenness on the skin of the face. But this skin property has different forms for everyone, and can be more or less noticeable.
The first signs of “stars” and “veins” can appear in childhood, and only competent treatment and maintenance of vascular health can protect against aggravation of the problem. If a girl has such a predisposition, then there is a chance that the rosacea network will become very noticeable after 30 years.
Treatment of rosacea on the skin of the face requires a systematic approach - regularly adding aromatic oils to your daily care - this will strengthen the walls of blood vessels and prevent their potential damage, for example, during stressful situations.
If the problem of rosacea already has a more pronounced condition, then the treatment procedure requires the use of hardware cosmetology:
- Photorejuvenation is the most popular method because it has no age restrictions. This procedure occurs under the influence of impulses, increases the regeneration of facial skin, and strengthens it. Subsequently, this makes the vascular network on the face invisible.
- Mesotherapy - the procedure ensures the supply of skin cells with a concentrated complex of useful substances, due to which minor defects, such as rosacea, disappear.
- Electrocoagulation is a procedure for removing large stars using electric current.
- The laser procedure will help remove pronounced vascular network.
- Ozone therapy is carried out only at an advanced stage of rosacea - during the procedure, damaged capillaries are removed under the influence of ozone oxygen using a microneedle.
An important knowledge in aesthetic cosmetology is also the structure of nervous tissue - the ectodermal formation of nerve cells, neurons. Its main task is the excitability and conductivity of nerve receptors and impulses from a specific organ to the central nervous system. They form a network of nerve nodes that perceive any irritation upon contact with them.
If the vascular or nervous system is damaged during the procedure, facial symmetry can be disrupted or a muscle or nerve may be pinched.
Knowledge of the location of the vascular and nerve networks on the face is a very important skill for a cosmetologist - when performing any injection technique, it is necessary to clearly understand where the ropes of large vessels and nerve tissues pass in order to avoid dangerous manipulations in these areas in the future.